If you've had diabetes for some time, you may have been carefully managing your blood sugar levels and watching your diet. Recently, though, you might have noticed something concerning, gums that bleed when you brush, a persistent dry mouth, or even loose teeth.
These symptoms aren't coincidental, diabetes and oral health are more closely connected than you might think. However, with proper care and attention, you can protect your mouth and maintain strong, healthy teeth, and gums.
What is diabetes?
Diabetes is a long-term condition that changes how your body handles blood sugar (glucose). To control and utilise these sugars, your pancreas usually produces insulin hormone. But, when diabetes develops, your body either doesn't make enough insulin or can't use it effectively.
There are three main types you should be aware of:
Type 1 diabetes:
Your immune system attacks the cells that make insulin. It usually develops in children or young adults and requires lifelong insulin treatment.
Type 2 diabetes:
Your body doesn't respond well to insulin, and over time, your pancreas may not produce enough. This type is more common in adults but is increasingly seen in younger people.
Gestational diabetes:
Gestational diabetes happens during pregnancy and usually goes away after childbirth, though it may increase your risk of developing type 2 diabetes later.
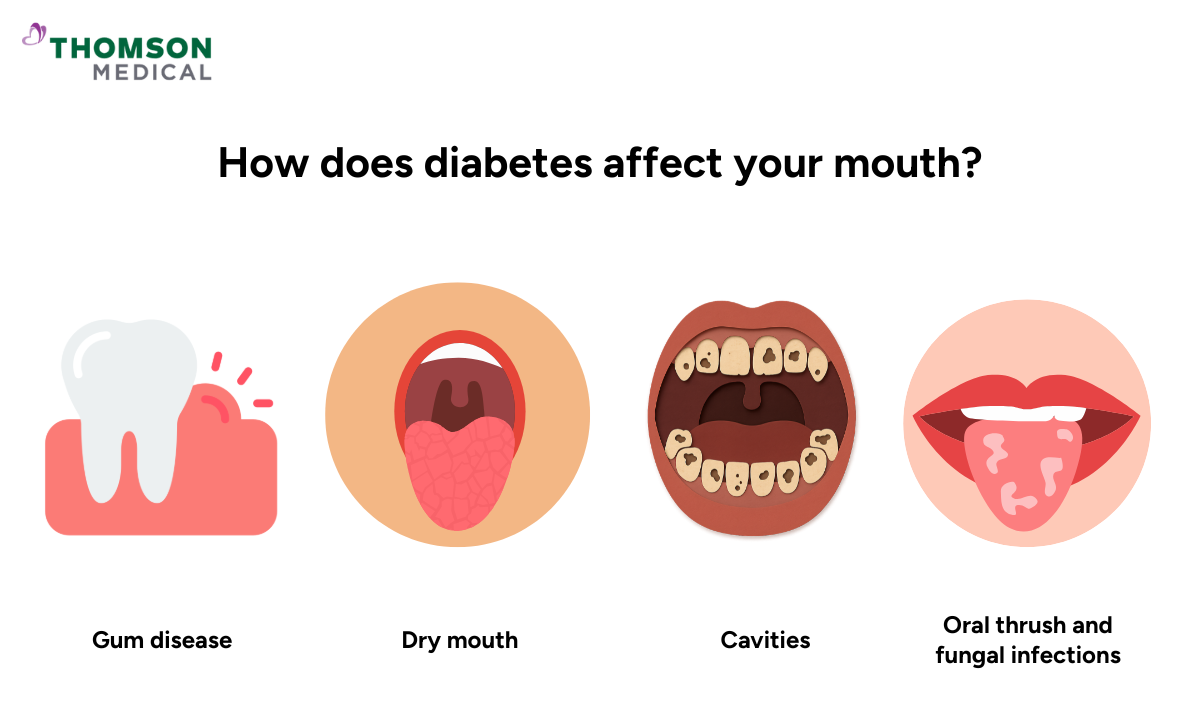
How does diabetes affect your mouth?
High blood sugar affects your whole body, including your mouth. When your blood glucose increases, it weakens your white blood cells. These cells normally protect you from infections, including those that develop in the mouth.
The link between diabetes and oral health works both ways. Diabetes can lead to oral health problems, and oral health problems can make diabetes harder to control.
Here's what you might experience:
| Oral health problem | What it is | What you should know |
|---|---|---|
| Gum disease (periodontal disease) | A periodontal disease is an infection and inflammation of the gums that can progress to affect the bone | Your gums may become red, swollen, or bleed easily. Healing may be slower, and severe gum disease can make blood glucose harder to control. |
| Dry mouth (xerostomia) | Reduced saliva flow | Can lead to difficulty swallowing, higher risk of decay, oral infections, and denture discomfort. |
| Cavities (tooth decay) | Damage to tooth enamel caused by acids from plaque bacteria | High blood sugar increases sugar in saliva, feeding bacteria that produce acids. Can cause pain, sensitivity, or tooth loss if untreated. |
| Fungal infections such as oral thrush | Overgrowth of Candida albicans in the mouth | May appear as white patches on the tongue or inside the mouth. High glucose levels make fungal growth easier. |
| Delayed wound healing | Slower repair of cuts, sores, and tissues in the mouth | Increases the chance of infections and prolongs recovery after dental procedures. |
| Changes in taste | Altered taste sensations, sometimes including metallic or burning sensations | Can affect enjoyment of food. Burning mouth syndrome may occur. |
| Higher chance of infections | Increased susceptibility to bacterial or recurrent oral infections | Weakened immunity can lead to abscesses, ulcers, or persistent infections. |
If you’re noticing any changes in your mouth or currently managing diabetes alongside oral symptoms, request an appointment with Thomson Medical. Our dentists can help you protect your oral health and support better overall wellbeing.
Our dentist and endocrinologist in Singapore
Loading...
Why is gum disease a concern when you have diabetes?
The connection between diabetes and gum disease runs both ways. When your blood sugar is high, there's more sugar in your saliva. Bacteria in your mouth feed on this sugar and produce acids that irritate your gums, causing gum inflammation. Over time, this can lead to gum disease.
The tricky part is that gum disease can also make it harder to control your blood glucose levels. Because when your gums are infected, your body has to work harder to fight the infection, which can cause your blood sugar to rise.
If gum disease isn't treated, the bone supporting your teeth can weaken, leading to loose teeth or even tooth loss. However, treating periodontal disease may help improve your blood glucose control over time.
What are the warning signs to watch for?
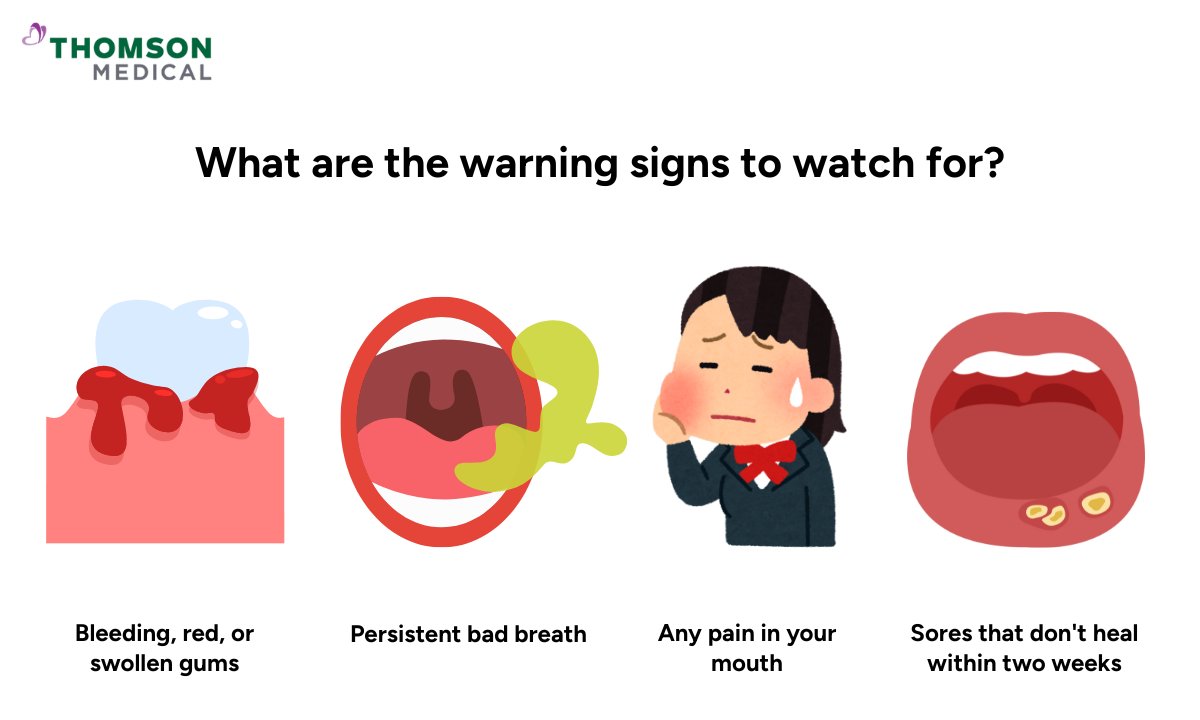
If you have diabetes, it's important to be aware of changes in your mouth. Contact your dentist if you notice any of the following:
Bleeding, red, or swollen gums
Gums pulling away from your teeth
Persistent bad breath that doesn't improve with brushing
Loose or shifting teeth
Any pain or discomfort in your mouth
Sores that don't heal within two weeks
What should you tell your dentist?
Open communication with your dentist is important for your oral health. Make sure to share:
That you have diabetes and what type
How well your blood sugar is currently controlled
All medicines you're taking, including insulin and any diabetes medicines
Any recent changes in your health or diabetes management
Any concerns you have about your oral health
Your dentist can work with your endocrinologist (diabetes specialist) to provide the best care for you. If you're planning to have dental treatment, let both your dentist and your endocrinologist know, especially if you're having oral surgery.
How can you keep your mouth healthy?
Taking care of your oral health while living with diabetes doesn't have to be complicated. Here are some practical steps you can take:
Control your blood sugar:
Keeping your blood sugar within your target range lowers your risk of gum disease and other oral health problems.
Brush and floss regularly:
Use a soft-bristled brush with fluoride toothpaste twice a day for 2 minutes.
Floss once a day to clean between your teeth where your brush can't reach.
See your dentist regularly:
Aim for at least two dental visits a year, or more frequently if your dentist recommends it.
Regular check-ups help catch dental problems early, when they're easiest to treat.
Manage dry mouth:
Drink water, chew sugar-free gum, or use saliva substitutes.
Your dentist can also recommend special mouth rinse products to help with dry mouth.
Staying hydrated and keeping your mouth moist helps prevent dental decay and keeps you comfortable.
Quit smoking:
Smoking makes it harder to control your blood sugar and significantly increases your risk of gum disease.
With good blood glucose control, a daily oral care routine, and regular dental check-up, you can reduce your risk of diabetes-related oral health issues. Even small improvements to your oral care routine can significantly impact your diabetes management.
If you have questions about dental care with diabetes, request an appointment at Thomson Medical. Our dentists and endocrinologist are ready to guide you, answer your questions, and support you with personalised care.
FAQ
Why is dental care so important for people with diabetes?
People with diabetes are at higher risk of oral health problems like gum disease, cavities, and dry mouth. These issues can make it harder to control blood sugar levels. Good dental care helps prevent these problems and supports your overall diabetes management.
How often should you visit the dentist if you have diabetes?
Most people with diabetes should see their dentist at least twice a year. However, if you have gum disease or other oral health issues, your dentist may recommend more frequent visits, perhaps every three to four months.
Why do people with diabetes get gum disease more easily?
When blood sugar is high, there's more sugar in your saliva. Bacteria feed on this sugar and produce acids that damage your gums. Additionally, high blood sugar weakens your immune system, making it harder for your body to fight gum infections.
How to manage dry mouth caused by diabetes?
Stay well-hydrated by sipping water throughout the day. Chew sugar-free gum or use sugar-free lozenges to help produce saliva. Your dentist may also recommend artificial saliva products or special mouthwashes. Avoid caffeine and alcohol, as these can make dry mouth worse.
Can gum disease affect your blood sugar control?
Yes, it can. Gum disease is an infection, and when your body fights an infection, it can cause your blood sugar to rise. This makes diabetes harder to control. The good thing is that treating gum disease can help improve your blood sugar levels.
Should you tell your dentist about your diabetes medications?
Absolutely. Your dentist needs to know all the medications you're taking, including insulin and other diabetes drugs. Some medications can affect your oral health or may need to be considered when planning dental treatment. Being open about your medications helps your dentist give you the safest, most effective care.
Is it safe to have dental procedures if you have diabetes?
Yes, dental procedures are generally safe for people with diabetes. However, it's important to coordinate with both your dentist and your diabetes care team, especially for more complex procedures. They'll help you manage your blood sugar levels before, during, and after treatment for the best outcome.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your conditions, request an appointment with Thomson Medical today.
