What is sciatica?
Sciatica is a term with several possible meanings. Medically speaking, sciatic nerve compression is an uncommon orthopaedic condition.
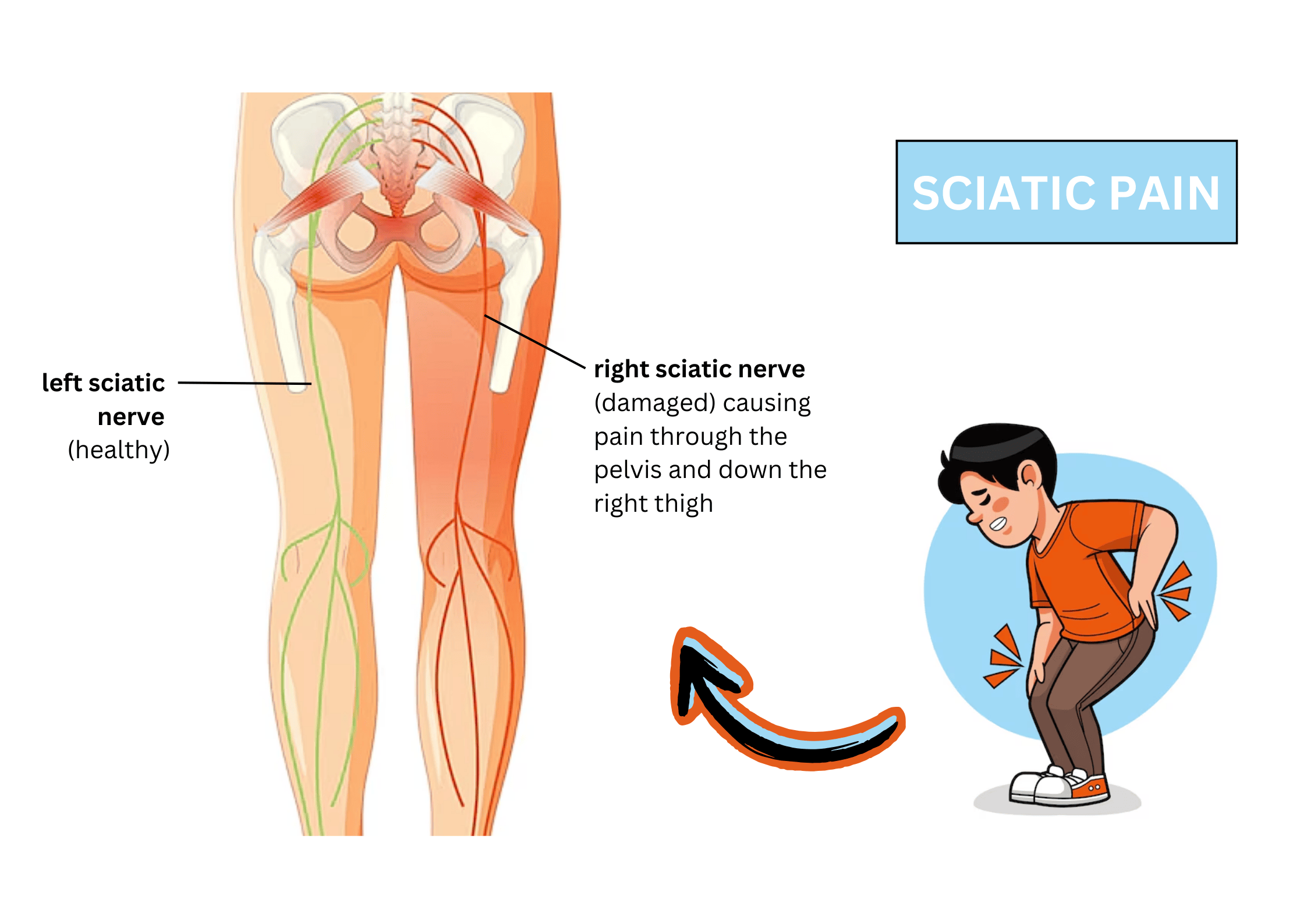
However, it is also commonly used to describe leg radicular pain, which is a general condition characterised by pain that extends from the lower back through the pelvis and down the back of one or both thighs. This is usually caused by the compression of the sciatic nerve, which is the largest nerve that runs along this region.
Sciatica is not a disease by itself, so if you are experiencing such pain, it might be a sign that you have an underlying condition. If your sciatic nerve is affected, you can experience anywhere between a mild ache to a sharp, burning sensation or excruciating discomfort on regular activities.
Types of Sciatica
There are two ways to classify different types of sciatica:
Acute vs. chronic sciatica
Short-term or acute sciatica is typically characterised by brief episodes of pain. If your sciatica is acute, some bed rest, over-the-counter medication, and gentle exercises may be enough to alleviate your symptoms.
On the other hand, chronic sciatica usually consists of consistent pain for a long period of time. It usually requires a more comprehensive treatment approach that combines pain relief medications, physiotherapy, and even spinal surgery.
Unilateral vs. bilateral sciatica
Sciatica typically affects the back of one leg, which suggests the condition is often unilateral rather than bilateral. However, sometimes both of your legs can be affected a condition known as bilateral involvement.
Causes and risk factors
Different conditions lead to the compression of the sciatic nerve. You need to look out for the following causes and risk factors that can contribute to sciatica:
Herniated disc
Herniated discs are the most common cause of sciatica. When the soft center of a spinal disc pushes through a crack in the tougher exterior, it can compress the sciatic nerve, leading to sciatic pain.
Bone spurs
Bone overgrowths (spurs) that form on the spine can compress certain nerves, including the sciatic nerve, which becomes the cause of pain and inflammation.
Spinal stenosis
Spinal stenosis is a condition that causes narrowing of the spinal canal, which happens often due to age-related conditions. This can put pressure on the sciatic nerve.
Spondylolisthesis
Spondylolisthesis occurs when one vertebra slips forward over another, pinching the sciatic nerve. Such a spinal injury can lead to pain in the spine, which radiates downward.
Piriformis syndrome
The piriformis muscle, located in the buttock region, can sometimes irritate or compress the sciatic nerve, causing radicular-like pain.
Trauma or injury
An injury to the lower back, such as from a fall, car accident, or sports-related injury, can lead to sciatica.
Tumours or infections
In rare cases, a tumour or infection in the spine can cause sciatica by pressing on the nerve root.
Symptoms of sciatica
You need to look out for pain that radiates from your lower spine to your buttocks and down the back of your leg. This is a hallmark symptom and is most likely to be a key diagnostic indicator for your healthcare provider.
Common symptoms of sciatica include:
Pain characteristics
A sharp, burning pain that radiates downwards from the spine to the affected leg. It is often exacerbated by prolonged sitting, standing, or sudden movements like coughing or sneezing.
Numbness and sensory changes
Tingling sensations, often described as needles and pins, are felt when the spinal nerves are compressed. This is often accompanied by numbness and is similar to the feeling experienced when the leg is asleep.
Muscle weakness
The presence of chronic muscle weakness is a sign of a more serious underlying issue. It usually manifests with additional symptoms like loss of bowel or bladder control, necessitating urgent care.
Experiencing any of the above symptoms? Don't delay seeking medical attention. Book an appointment with Thomson Medical's specialists for a comprehensive assessment and personalised treatment plan.
Diagnosis of sciatica
Your healthcare professional will start by taking your medical history. It is essential to discuss any previous injuries or health conditions that might relate to your current symptoms during this phase.
If sciatica is suspected, they will then move on to further evaluation, which may involve:
Physical examination techniques
The doctor will test your muscle strength and reflexes to identify the source of pain. Your ability to perform physical activities like walking on your toes or raising your leg while lying down (straight leg raise test) will also be evaluated during your physical exam.
Imaging and diagnostic tests
X-rays:
They help detect bone spurs or other spinal issues.
Magnetic resonance imaging (MRI):
An MRI scan provides detailed images of soft tissues, including herniated discs or nerve compression.
CT scans:
A CT scan may be used with a contrast dye to get a better view of the spinal cord and nerves.
Electromyography (EMG):
It measures electrical impulses in the muscles and nerves to identify nerve damage.
Treatment for sciatica
Sciatica typically improves with time and self-care measures, although some cases may require more intensive treatment. If you have sciatica, the healthcare provider will focus more on relieving pain and addressing the underlying cause.
Self-care and home remedies
Rest:
Short periods of rest can help relieve pressure on the sciatic nerve and provide short-term relief, but prolonged inactivity should be avoided.
Cold and heat therapy:
Applying cold packs to the affected area for 15–20 minutes several times a day can reduce inflammation. After a few days, heat packs may help relax tense muscles.
Over-the-counter painkillers:
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or Arcoxia can reduce inflammation and pain.
Medications for pain relief
Prescription pain relievers:
In more severe cases, doctors may prescribe stronger pain medications, including muscle relaxants or anti-inflammatory drugs.
Corticosteroid injections:
A corticosteroid injection near the irritated nerve root can reduce inflammation and provide temporary relief from severe pain.
Antidepressants or anti-seizure medications:
These medications can help relieve chronic nerve pain associated with sciatica.
Physical therapy and rehabilitation
Stretching exercises:
A physical therapist can recommend specific regular exercises to stretch the muscles around the sciatic nerve, such as the hamstrings and piriformis.
Core muscle strengthening exercises:
Strengthening the core and back muscles can help support the spine and relieve pressure on the sciatic nerve.
Posture training:
Learning proper posture techniques for sitting, standing, and lifting can prevent further aggravation of the sciatic pain.
Surgery
Microdiscectomy:
In cases where a herniated disc is compressing the sciatic nerve, a surgeon may remove part of the disc to relieve pressure.
Laminectomy:
This involves removing part of the vertebra (the lamina) to create more space and reduce pressure on the sciatic nerve.
Spinal Fusion:
Some patients with sciatica get spinal instability. In this case, surgeons go for a spinal surgery where they fuse two vertebrae together to stabilise the spine.
Alternative Therapies
Chiropractic Care:
Spinal adjustments may help reduce sciatica nerve irritation and improve mobility.
Acupuncture:
Acupuncture is a traditional Chinese medicine technique that involves inserting thin needles into specific points on the body to relieve sciatica pain.
Massage Therapy:
Therapeutic massage may help relax muscles and relieve pressure on the sciatic nerve.
Prevention strategies for sciatica
If you have a risk of developing sciatica, there is still a way to prevent the symptoms from worsening. To prevent sciatica, you need to embrace a healthier lifestyle with habits such as:
Exercise regularly:
Strengthening your core muscles can help support your spine and lower the risk of sciatica.
Practice good posture techniques:
Maintain good posture when sitting, standing, and lifting heavy objects to minimise stress on your lower back and prevent nerve damage.
Avoid prolonged sitting:
Instead of sitting for longer periods, take breaks to stand up, stretch, and walk around, which can help make sciatica preventable.
Maintain a healthy weight:
Having a healthy body weight can relieve the pressure on your spine, decreasing the occurrence of potential risk factors.
Proper lifting techniques:
When lifting, use your legs rather than your back and avoid twisting motions that can strain the lumbar spine.
Disclaimer: The information provided is for general knowledge only and should not be considered a substitute for professional medical advice. If you are concerned about having sciatica, you can request an appointment with our specialists at Thomson Medical for an accurate diagnosis and tailored treatment plan.
Sciatica Specialists in Singapore
Loading...
Frequently Asked Questions (FAQs)
What is the most common cause of sciatica?
A herniated disc is the most common cause of sciatica. It occurs when the soft interior of a spinal disc pushes through its tough exterior and compresses the sciatic nerve.
How long does sciatica take to heal?
In most cases, sciatica improves within 4 to 6 weeks with proper treatment. However, chronic sciatica or severe cases may take longer to heal or require more intensive interventions.
Is sciatica a permanent condition?
Sciatica is usually not a permanent condition. With proper treatment, most people recover fully. However, if the underlying cause is not treated properly or if there is permanent nerve damage, sciatica can become a long-term problem.
When should I see a doctor for sciatica?
You should see a doctor if you experience severe or worsening pain, weakness or numbness in the leg; loss of bladder function or bowel control; or if there is severe pain for more than a few weeks despite home treatments.
Can exercise make sciatica worse?
Certain high-impact or strenuous exercises can worsen sciatica symptoms. However, gentle stretching and low-impact activity, like walking or swimming, can help alleviate chronic pain.
Can sciatica be cured?
Sciatica can be effectively treated and managed in most cases. The key is addressing the underlying cause of nerve compression and following a comprehensive treatment plan, which may include physical therapy, medical therapy, and lifestyle changes.
What is the best sleeping position for people with sciatica?
Sleeping on your back with a pillow under your knees or sleeping on your side with a pillow between your knees can help reduce pressure on the sciatic nerve and alleviate pain.
Can weight loss help with sciatica?
Yes, losing excess weight can reduce pressure on the spine and lower back, which may help relieve sciatica symptoms and prevent future episodes.
What are the risk factors for sciatica?
Risk factors include age (due to degenerative changes in the spine), obesity, a sedentary lifestyle, prolonged sitting, occupations that require heavy lifting, and diabetes (which increases the risk of nerve damage).
Can chiropractic care help with sciatica?
Yes, chiropractic adjustments may provide relief from sciatica symptoms by reducing nerve irritation and improving spinal alignment. However, it is important to consult with a healthcare professional to determine the best course of treatment.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, please consult a specialist at Thomson Medical. Book an appointment with Thomson Medical today.
For more information, contact us:
Thomson Medical Concierge
- 8.30am - 5.30pm
- WhatsApp: 9147 2051
Need help finding the right specialist or booking for a group?
Our Medical Concierge is here to help you. Simply fill in our form, and we'll check and connect you with the right specialist promptly.
Notice:
The range of services may vary between Thomson clinic locations. Please contact your preferred branch directly to enquire about the current availability.
Get In TouchDr Jerry Chen
Orthopaedic Surgery
Thomson Specialists (Thomson Medical Centre)
English, Mandarin, Cantonese, Hokkien
Income, Great Eastern, AIA, Singlife and 4 others

.png%3Fbranch%3Dprod&w=3840&q=75)