What is polycystic ovary syndrome (PCOS)?
Polycystic Ovary Syndrome (PCOS) is a hormonal problem for women of reproductive age.
When you have PCOS, you may:
Have irregular or missed periods
Produce higher levels of male hormones (called androgens)
Develop small fluid-filled sacs (cysts) on the ovaries
This condition affects about 1 in 10 people with ovaries and may contribute to infertility. However, with the right management, most women with PCOS can lead healthy lives and conceive successfully.
How do hormones affect PCOS?
Hormones are chemical messengers of your body that travel in your blood to tell different parts of your body what to do. These chemical signals control many important functions, from your appetite to your reproductive cycle.
The ovaries produce both female (oestrogen and progesterone) and small amounts of male hormones (testosterone). In PCOS, this balance shifts, causing problems with ovulation and hormone levels.
This can cause effects including:
Your body may become resistant to insulin, leading to higher insulin levels.
Increased insulin levels stimulate your ovaries to excessively produce testosterone.
The excess testosterone interferes with normal ovary function, due to which eggs may not develop properly or be released during your cycle;
As a result of these hormonal imbalances, cysts may form on the ovaries.
The name "polycystic ovarian syndrome" comes from the multiple small cysts that often develop on the ovaries. However, not everyone with PCOS has visible cysts, and the condition can still be diagnosed based on other factors.
Causes of PCOS
The exact cause of PCOS is not fully understood, but it is believed to be influenced by both genetic and environmental factors.
Hormonal Imbalances
Women with PCOS often have higher levels of androgens and insulin resistance, which can interfere with ovulation.
Genetics
A family history of PCOS can increase the likelihood of developing the condition, indicating a genetic component to its occurrence.
Insulin Resistance
Many individuals with PCOS exhibit insulin resistance, which means their cells do not respond effectively to insulin. This condition can lead to higher insulin levels, contributing to weight gain and increased production of androgens.
Signs and symptoms of PCOS
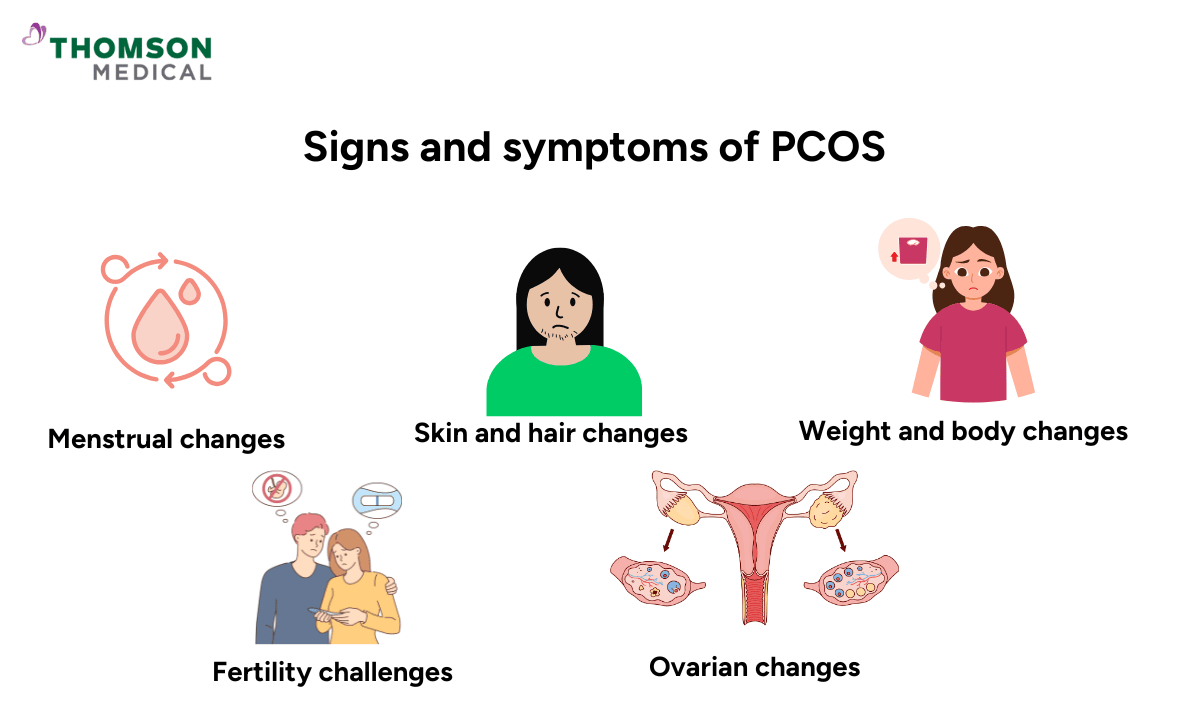
PCOS manifests differently in different women, with variations in symptoms, severity, and health impacts.
Some may experience irregular periods and fertility challenges, while others might face issues like acne, excessive hair growth, or weight gain, depending on the hormonal imbalances and other factors unique to their condition.
Menstrual changes
Irregular periods that come infrequently or unpredictably
Very heavy or very light bleeding
Missed periods that can last months
Skin and hair changes
Extra hair growth on your face, chest, back, or abdomen
Persistent acne that may not respond to typical treatments
Thinning hair or patches of hair loss on your scalp
Weight and body changes
Weight gain, especially around your middle
Difficulty losing weight despite healthy eating and exercise
Darker, thickened skin patches (especially in neck creases, armpits, or under breasts)
Fertility challenges
Trouble getting pregnant due to irregular or absent ovulation
You have a higher risk of pregnancy complications if you do conceive
Ovarian changes
Small fluid-filled sacs (cysts) may develop on your ovaries
Not everyone with PCOS has visible cysts on ultrasound
Many of these symptoms can be managed effectively with proper treatment.
If you're experiencing symptoms of PCOS, talking to a healthcare provider is a great first step. Request an appointment with Thomson Medical for a comprehensive evaluation. Our specialists may recommend a pelvic ultrasound to accurately assess your condition and create a personalised treatment plan. Be sure to follow any preparation guidelines and discuss all concerns with your gynaecologist to ensure the most accurate results.
Diagnosing PCOS
Diagnosing PCOS generally involves several steps:
Medical history
A healthcare provider will assess your medical history, focusing on symptoms such as irregular menstrual cycles, weight gain, and excessive hair growth.
Physical examination
The doctor will conduct a physical exam to identify signs of hirsutism (excessive hair growth), acne, and obesity.
Blood tests
Your doctor may order blood tests to check for hormone imbalances or insulin resistance. These tests help confirm PCOS and rule out other conditions that might cause similar symptoms.
Ultrasound
Pelvic ultrasound is essential for diagnosing PCOS, as it provides a detailed view of the ovaries, detecting multiple small follicles and enlargement. However, the presence of cysts alone is not enough for diagnosis. Doctors also assess symptoms, blood tests, and medical history to confirm PCOS.
PCOS ultrasound scan vs. normal ultrasound
PCOS ultrasound
During a pelvic ultrasound for PCOS, the technician specifically looks for the presence of multiple small cysts—typically 12 or more—located along the periphery of the ovaries.
These cysts represent immature follicles that did not ovulate, a characteristic feature of PCOS. Additionally, the ovaries may appear enlarged during this examination.
Normal ultrasound
Conversely, a standard pelvic ultrasound is used to assess your reproductive organs for various conditions, such as fibroids, endometriosis, or other cysts unrelated to PCOS.
In this type of ultrasound, the ovaries generally do not show signs of enlargement, and there is no distinct pattern of cysts observed.
What are antral follicles?
Antral follicles are small, fluid-filled sacs in the ovaries that contain immature eggs. They are visible during a pelvic ultrasound and are part of the normal ovarian cycle.
During a menstrual cycle, several antral follicles develop, but typically only one matures and releases an egg during ovulation.
In women with PCOS, many antral follicles develop but do not mature properly. This leads to the formation of cysts on the ovaries, which is a key feature that doctors look for when diagnosing PCOS through ultrasound.
Cysts vs. follicles in PCOS
Cysts and follicles are different, although they can appear similar on an ultrasound.
Feature | Follicles | Cysts |
Definition | Small, fluid-filled sacs in the ovaries that contain immature eggs and are part of the normal reproductive process. | Enlarged sacs form when follicles fail to release an egg and continue to grow. |
Size | Typically 2–5 mm in diameter. | Usually larger, often greater than 10 mm in diameter. |
Function | Grow and mature during a normal cycle, releasing eggs during ovulation. | Do not release eggs; instead, accumulate along the edges of the ovaries in PCOS. |
Appearance in PCOS | Multiple follicles develop but fail to mature, leading to cyst formation. | Cysts create a "string of pearls" pattern on ultrasound and may cause the ovaries to appear enlarged. |
Normal cycle role | Essential for ovulation and egg release. | This condition is not part of a normal cycle; it results from disrupted ovulation in PCOS. |
How is PCOS treated?
PCOS can be managed through a combination of lifestyle changes, home remedies, and medications. Below is a detailed look at how PCOS is treated.
Lifestyle and home remedies
The first step to managing PCOS is to change your lifestyle. By adopting healthy habits, you can improve symptoms and promote hormonal balance. They also lower the risk of serious issues like diabetes and heart disease.
Weight management
Maintaining a healthy weight can help you regulate insulin levels and improve hormonal imbalances associated with PCOS.
Diet
Following a balanced diet that includes low glycaemic index foods can assist in managing insulin resistance and maintaining stable blood sugar levels.
Exercise
Simple activities, like walking for 30 minutes a day or practicing yoga, can improve insulin sensitivity and overall well-being.
Stress management
Mindfulness practices such as meditation or deep breathing exercises can help reduce stress levels, promote emotional well-being, and support hormonal balance.
Medications
In addition to lifestyle changes, medications may be prescribed to help manage the symptoms of PCOS. Depending on the severity of the condition and the symptoms experienced, doctors may recommend you the following:
Birth control pills
These are often prescribed to regulate menstrual cycles, lower androgen levels, and manage symptoms like acne and hirsutism.
Metformin
This medication is commonly used to treat insulin resistance in PCOS. It improves insulin sensitivity and may promote ovulation.
Clomiphene (Clomid)
A fertility medication that stimulates ovulation in women with PCOS who are trying to conceive.
Anti-androgens
Medications such as spironolactone can help reduce excessive hair growth and acne by blocking the effects of excess male hormones.
Progestin therapy
For those who prefer not to use birth control pills, progestin can help regulate menstrual cycles.
These are just a few of the ways PCOS can be treated. It's important to remember that the best approach to managing PCOS will vary from person to person.
A healthcare provider will help tailor treatment plans based on individual symptoms and goals, whether it’s regulating periods, managing fertility, or addressing other concerns such as acne and weight gain.
FAQ
What are the warning signs of PCOS?
The warning signs of PCOS can vary, but some common symptoms to look out for include:
Irregular periods
Women may experience periods that are infrequent, absent, or excessively long. Some women may have fewer than eight periods per year or may skip them altogether.
Excess hair growth (hirsutism)
There is an increase in hair on the face, chest, abdomen, or back due to high levels of androgens (male hormones).
Acne
Increased pimples or oily skin, often seen along the chin, jawline, and neck, caused by hormonal imbalances.
Thinning hair or male-pattern baldness
There is thinning of hair on the scalp or a receding hairline.
Weight gain
Difficulty losing body weight or significant weight gain, often due to insulin resistance.
Infertility
The woman is having trouble getting pregnant due to irregular ovulation or lack of ovulation.
Darkened skin
Acanthosis nigricans is characterised by patches of dark, thickened skin, often in areas like the neck, underarms, and groin.
Pelvic pain
Some women with PCOS may experience pelvic pain or discomfort, especially if they have cysts on their ovaries.
How to confirm PCOS?
To confirm PCOS, doctors typically perform a combination of the following steps:
Medical history and symptoms
The doctor will review your menstrual cycle, symptoms of excess hair growth, acne, or weight gain, and ask about your overall health.
Physical exam
A physical examination may include checking for signs like excess hair growth (hirsutism) or acne.
Blood tests
Blood tests are used to check hormone levels (like androgens, insulin, and other relevant hormones) to rule out other conditions. Elevated levels of androgens or insulin resistance are common indicators of PCOS.
Pelvic ultrasound
A transvaginal ultrasound or pelvic ultrasound may be performed to look for multiple small cysts on the ovaries. In PCOS, the ovaries often show a "string of pearls" appearance due to the presence of immature follicles.
For a diagnosis of PCOS, doctors typically use the Rotterdam criteria, which require at least two of the following:
Irregular or absent periods
Excessive androgen levels (clinical signs like hirsutism or lab results showing high androgen levels)
Ovarian cysts (on ultrasound)
What indicates PCOS on an ultrasound?
Multiple small cysts (follicles)
The ovaries may contain 12 or more small follicles (2-9 mm in size) that are clustered around the outer edge of the ovary, creating a characteristic "string of pearls" appearance.
Enlarged ovaries
The ovaries may appear enlarged (usually greater than 10 mL in size), and the follicles within may prevent the ovaries from releasing an egg (ovulation).
Thickened ovarian capsule
In some cases, the outer shell (capsule) of the ovary may appear thicker than normal.
Is PCOS a serious problem?
PCOS is generally not life-threatening, but it can lead to various health complications if not managed properly. Some of the serious risks and issues associated with PCOS include:
Infertility
PCOS is one of the leading causes of infertility in women, as it can interfere with normal ovulation.
Type 2 diabetes
Many people with PCOS have insulin resistance, which can increase the risk of developing type 2 diabetes.
Heart disease
Due to insulin resistance and higher levels of cholesterol and blood pressure, individuals with PCOS may have a higher risk of cardiovascular disease.
Endometrial cancer
If menstruation is infrequent or absent for long periods, the condition can increase the risk of uterine (endometrial) cancer due to the thickening of the uterine lining.
Mental health issues
Women with PCOS may be at a higher risk for anxiety, depression, or eating disorders due to the emotional toll of managing symptoms like weight gain, hirsutism, and infertility.
How to check PCOS at home?
While a definitive diagnosis of PCOS requires medical consultation and tests, there are some at-home signs you can monitor:
Track menstrual cycles
Keep track of your periods. If they are very irregular (more than 35 days apart) or absent for several months, it may be a sign of PCOS.
Watch for excess hair growth
Keep track of any unusual or excessive hair growth, especially in areas like the face, chest, or abdomen, which could be a sign of higher androgen levels.
Monitor skin changes
If you notice persistent acne or oily skin, especially in areas like the chin or jawline, it could be a sign of hormonal imbalance.
Notice weight changes
If you're gaining weight or struggling to lose weight despite eating a balanced diet and exercising, these symptoms could be linked to insulin resistance, a common issue in PCOS.
Pelvic pain or discomfort
Pay attention to any ongoing pelvic pain, especially if it occurs along with irregular periods or difficulty getting pregnant.
When is the best time to do an ultrasound for PCOS?
What to expect during a follicular scan?
If you're feeling nervous about a transvaginal ultrasound, knowing what to expect can help ease your concerns. Here's a step-by-step guide:
No need for a full bladder
Unlike abdominal ultrasounds, a full bladder is not required for a follicular scan. In fact, having an empty bladder provides a clearer view of the ovaries.
Use of a transvaginal probe
A thin, wand-shaped ultrasound probe is gently inserted into the vagina. This allows for detailed imaging of the ovaries and developing follicles, offering more accuracy than an abdominal scan.
Comfort and lubrication
The probe is lubricated before insertion to ensure comfort. Try to stay relaxed and take slow, deep breaths. If you experience any discomfort, inform your technician immediately.
Mild pressure, but minimal pain
You may feel some pressure as the probe moves inside to capture images, but the procedure should not be painful. If needed, you can ask for a break during the scan.
Scanning the ovaries
The technician will carefully move the probe to examine the ovaries and measure the follicles. The scan typically lasts 10–15 minutes.
Getting your results
After the scan, your healthcare provider will review the findings and explain what they mean. You will also receive a final report with detailed measurements. Don’t hesitate to ask questions about your results.
While a transvaginal scan may feel slightly uncomfortable, it provides valuable insights for women tracking ovulation, managing PCOS, or trying to conceive.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your medical conditions, request an appointment with Thomson Medical.
For more information, contact us:
Thomson Specialists Paragon (Health Screening)
- Mon - Fri: 8.30am - 5.30pm
- Sat: 8.30am - 12.30pm
Call: 6735 0300
Request a Health Screening