You might have noticed something's different, maybe an unusual odor or a change in your discharge. It's completely natural to feel concerned when your body signals that something's off, especially when it involves such a private area.
Bacterial vaginosis is more common than you might think, affecting countless women just like you. Knowing what's happening can bring relief and help you take the next steps with confidence.
What is bacterial vaginosis?
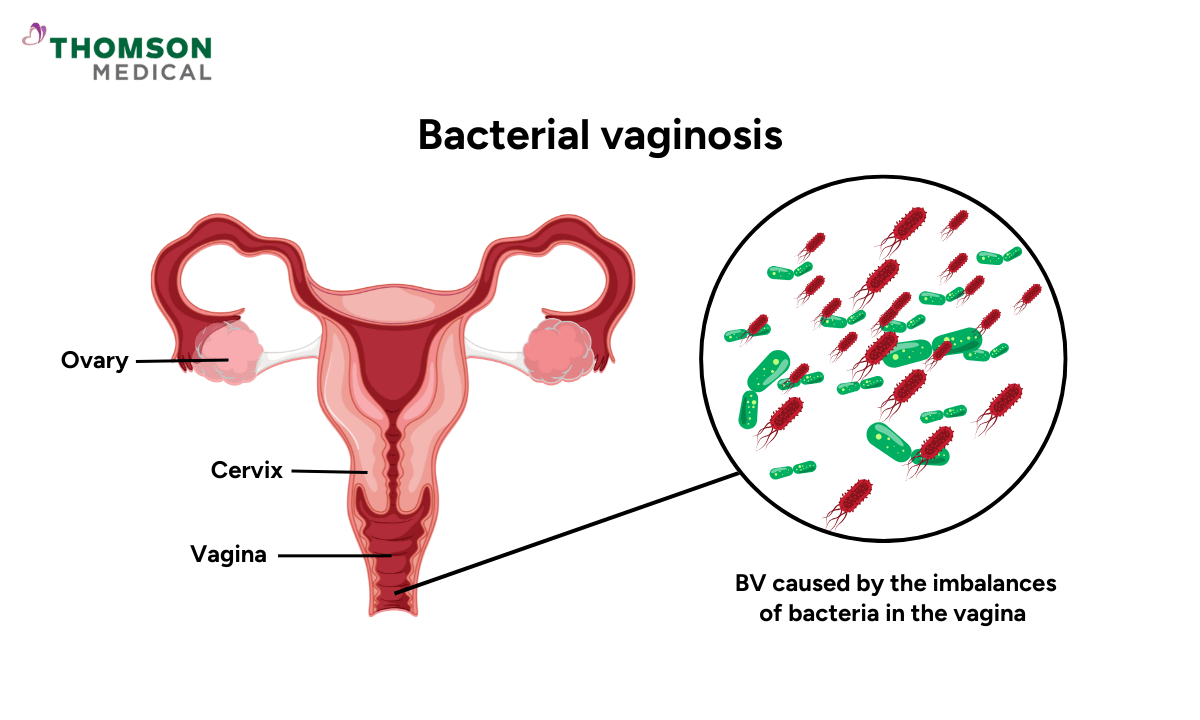
Bacterial vaginosis, or BV, happens when the balance of bacteria in your vagina gets disrupted. Think of your vagina as having its own ecosystem of bacteria. Some are helpful, while others can cause problems if they grow too much.
When you have BV, the good bacteria (called Lactobacillus) decrease, while harmful bacteria multiply. This imbalance can lead to symptoms like abnormal discharge, odor, and irritation.
What causes bacterial vaginosis?
We don't fully understand why BV develops, but it involves a shift in your vaginal environment. Normally, beneficial Lactobacillus bacteria, particularly Lactobacillus crispatus, keep your vagina slightly acidic, which prevents harmful bacteria from taking over.
When these good bacteria decrease, harmful bacteria can overgrow and create the bacterial imbalance that we call BV. The healthy vaginal flora produces hydrogen peroxide, which naturally protects against harmful bacteria.
Types of bacterial vaginosis based on symptoms
There are different types of bacterial vaginosis depending on how the symptoms appear and progress.
Acute BV
This type appears suddenly with noticeable symptoms like increased vaginal discharge with a fishy smell, itching, and irritation. These symptoms come on quickly and are usually the first sign that something's changed.
Recurrent BV
Sometimes BV returns shortly after you've finished treatment. If you're experiencing this, it's important to follow up with your doctor so we can work together to find a treatment approach that works better for your body.
Our specialist
Loading...
What are the signs and symptoms of bacterial vaginosis?
Many women with BV don't notice any symptoms at all. But when symptoms do appear, here's what you might experience:
Thin and watery vaginal discharge
Grayish-white or greenish vaginal discharge
Fishy vaginal odor
Vaginal itching or irritation
Burning during urination
Discomfort or pain during sexual intercourse
Because BV symptoms can look similar to other vaginal infections, it's important to visit your doctor for a proper diagnosis rather than trying to self-diagnose.
If you’re experiencing any of these symptoms or notice changes in your vaginal discharge or odor, request an appointment with Thomson Medical. Our women’s health specialists can provide an accurate diagnosis, explain the cause, and recommend the right treatment to help you feel comfortable again.
Who can get bacterial vaginosis?
Anyone with a vagina can develop bacterial vaginosis. It most commonly occurs in people who are sexually active, though it's rare in those who've never had sex.
Your risk of developing BV may be higher if you:
Are pregnant
Engage in unprotected sex without condoms or dental dams
Have an intrauterine device (IUD, a T-shaped contraceptive device placed in your uterus)
Have multiple or new sex partners
Use douches (liquid solutions used to rinse the vagina)
Are taking antibiotics
What's the difference between bacterial vaginosis and a yeast infection?
Both BV and yeast infections are vaginal infections that cause increased discharge, but they're quite different:
Feature | Bacterial vaginosis (BV) | Yeast infection |
Discharge | Thin, watery discharge with a distinct fishy smell | Thick and white, similar to cottage cheese; usually doesn't smell strong |
Vaginal irritation | Typically doesn't cause much itchiness or irritation | Often causes itchiness and irritation |
Treatment | Requires a doctor visit and prescription antibiotics | Can be treated with over-the-counter medications |
How bacterial vaginosis is diagnosed
To diagnose bacterial vaginosis, your doctor will ask about your medical history and perform a pelvic exam. During the pelvic exam, your provider will place gloved fingers inside your vagina to look for signs of infection, like an increase in discharge or foul-smelling discharge that has a white or gray color.
They'll take a sample of your vaginal discharge to test for bacteria and may check your vaginal pH level.
How to get tested for bacterial vaginosis?
If your doctor suspects BV, they'll take vaginal swabs for testing. These samples are sent to a lab where specialists can identify what type of infection you have.
For women who are sexually active, your doctor may recommend additional testing to rule out sexually transmitted diseases like chlamydia and gonorrhoea, since the symptoms can sometimes overlap. Common BV tests include:
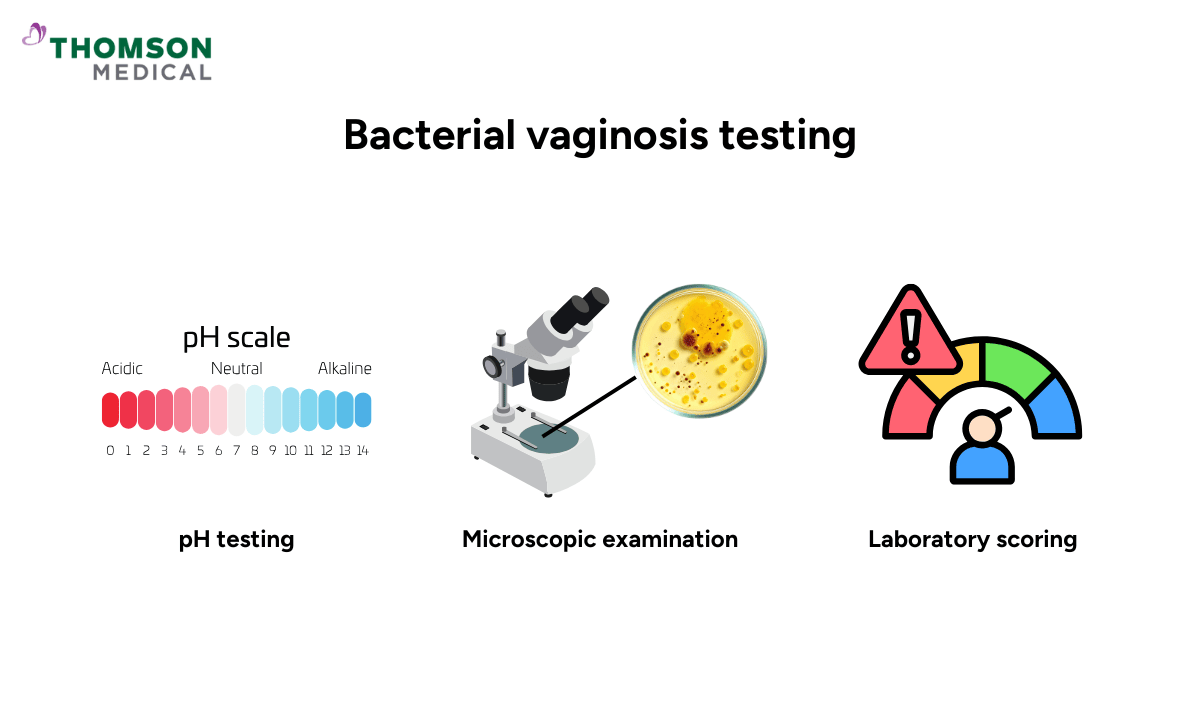
pH testing
One key indicator of BV is a high vaginal pH level
Your vagina is normally slightly acidic, but with BV, the pH of vaginal fluid becomes less acidic, typically rising above 4.5
Microscopic examination
Wet mount test where vaginal fluids are examined under a microscope to look for clue cells and bacteria
Gram stain used to examine the bacteria present in your vaginal fluids and identify specific types
Laboratory scoring
Nugent score, a standardized system that evaluates the types and amounts of bacteria to confirm BV (scores range from 0-10, with 7-10 indicating BV)
How is bacterial vaginosis treated?
Treatment for BV focuses on eliminating the overgrowth of harmful bacteria. Your doctor will prescribe antibiotics, which can come in different forms:
Oral antibiotics like metronidazole or tinidazole
Intravaginal antibiotics that are applied directly inside the vagina, such as metronidazole gel or clindamycin cream
In some cases, your doctor might suggest probiotics or lactobacillus supplements alongside antibiotics to help restore the balance of good bacteria in your vagina.
What are the potential complications of bacterial vaginosis?
BV doesn't cause complications very often, but leaving it untreated can sometimes lead to:
Increased risk of sexually transmitted infections like HIV, herpes, chlamydia, or gonorrhoea
Pelvic inflammatory disease (PID), an infection of your uterus and fallopian tubes that can affect fertility
Higher risk of infection after gynaecological procedures
Increased risk of preterm birth or low birth weight in pregnant women
How to prevent bacterial vaginosis
While we can't prevent BV entirely, there are steps you can take to reduce your risk:
Avoid scented products and harsh soaps and washing your genital area with warm water
Rinsing with water during regular bathing is enough to maintain its balance.
Use latex condoms or dental dams during sexual activity
When should you see a doctor?
Make an appointment with your doctor if:
Your vaginal discharge smells unusual and you're experiencing discomfort
You've had vaginal infections before but your discharge seems different this time
You have a new or different sex partner
You thought you had a yeast infection but still have symptoms after trying over-the-counter treatment
If you’re noticing any of these changes or ongoing discomfort, don’t ignore the signs. Request an appointment with Thomson Medical to get a proper diagnosis and the right treatment. Our specialists can help identify the cause and ensure your vaginal health is well cared for.
FAQ
Who is at risk of bacterial vaginosis?
Having multiple or new sex partners can disrupt your vaginal balance. Engaging in unprotected sex, using vaginal douches, smoking, and hormonal changes during pregnancy or menopause can affect your vaginal flora. Certain medications like antibiotics or corticosteroids may also increase risk.
Can bacterial vaginosis be cured?
Yes, bacterial vaginosis can be effectively treated and cured with proper medical care. It's essential to take the full course of antibiotics your doctor prescribes, even if symptoms improve early. This ensures complete elimination and reduces recurrence risk.
What are the complications of bacterial vaginosis?
Bacterial vaginosis typically doesn't cause complications when treated promptly. However, if left untreated, it can increase your risk of sexually transmitted infections, lead to pelvic inflammatory disease (which can affect fertility), cause pregnancy complications, or result in infections after gynecologic procedures.
What are the impacts of bacterial vaginosis on sexual health?
Bacterial vaginosis can cause discomfort or pain during sex due to vaginal irritation or inflammation. Treating BV symptoms and restoring your vaginal health can improve sexual function and intimacy. While BV isn't considered a sexually transmitted infection, male partners of women with recurrent bacterial vaginosis may carry the bacteria, so your doctor might consider partner treatment to reduce the risk of reinfection.
Can men get bacterial vaginosis?
No, men cannot get bacterial vaginosis because BV is specific to the vaginal environment. However, men can carry the bacteria that cause BV and potentially spread them to female partners, which can lead to the infection recurring in women.
Can a woman give another woman bacterial vaginosis?
Yes, bacterial vaginosis can spread between female sex partners through sexual activity. Since BV can be transmitted this way, both partners may need treatment if one is experiencing symptoms.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
