You may have first noticed unusual vaginal discharge, pelvic discomfort, or pain during intercourse, which these symptoms may seem minor at the time. When these signs persisted, a medical check-up may have revealed findings linked to cervical cancer or ovarian cancer.
It’s natural to wonder whether these two types of gynaecological cancers are related, and how having one may affect your overall risk. While both can share similar symptoms, they arise from different parts of the reproductive system. Understanding the key differences between cervical and ovarian cancer, including how they develop, their symptoms, and ways to detect them can help you take informed steps towards timely evaluation and care.
What is cervical cancer?
Cervical cancer is a type of cancer that grows on the cervix, the lower part of the womb that connects to the vagina. The human papillomavirus (HPV), a sexually transmitted infection (STI), is the main cause of cervical cancer.
Types 16 and 18 of HPV are high-risk strains that can cause infections that last a long time and lead to precancerous lesions and cervical cancer. Cervical cancer usually grows slowly, starting with abnormal changes in cervical cells called cervical dysplasia. These changes can be found and treated before they turn into cancer.
Risk factors for cervical cancer
While most cervical cancers are caused by HPV, other factors can also increase your risk of developing the disease. These include:
Having multiple sexual partners, which increases the risk of HPV infection
Smoking, which weakens the immune system, making it harder to fight off HPV
Weakened immune system due to HIV or other conditions that compromise immunity
Lack of regular check-ups that allow precancerous changes to go undetected
How to protect yourself
Although cervical cancer can be concerning, it's also treatable when found in the early stages. However, since cervical cancer often doesn't produce symptoms until it's advanced, prevention is your best defense. Here's how you can protect yourself:
Practicing safe sex to reduce HPV exposure
Get regular screenings including Pap smears and HPV test
Consider HPV vaccination for additional protection
What is ovarian cancer?
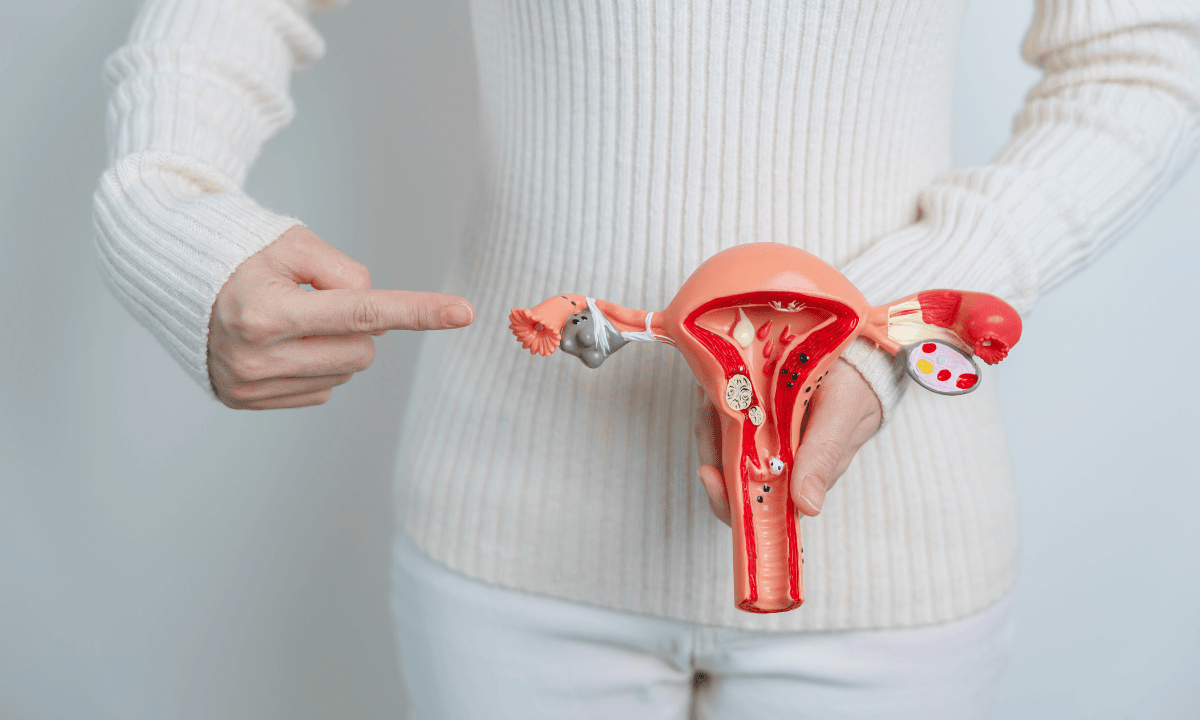
Ovarian cancer happens when abnormal cells in the ovaries grow and multiply in an uncontrolled way. The ovaries are almond-sized organs located on either side of the womb. They are responsible for producing eggs and hormones, such as oestrogen and progesterone.
Although the exact cause of ovarian cancer is not fully understood, especially in comparison to cervical cancer, certain risk factors may increase your likelihood of developing the condition:
Family history of ovarian or breast cancer:
Having relatives diagnosed with ovarian or breast cancer may indicate a genetic predisposition for ovarian cancer.
Genetic mutations:
Mutations in the BRCA1 and BRCA2 genes significantly increase the likelihood of ovarian cancer.
Age:
Most cases of ovarian cancer occur in women over 50, especially after menopause.
Reproductive history:
Women who haven't had children or who started menstruation early and entered menopause late may be at higher risk.
Hormone therapy:
Long-term use of hormone replacement therapy may increase the risk of ovarian cancer.
How to protect yourself
Currently, there is no guaranteed way to completely prevent ovarian cancer. However, there are steps you can take to protect your health:
Being aware of your family's history of ovarian cancer
Get regular ovarian cancer screening to help find and treat the disease early
If you are at high risk, genetic testing and preventive surgeries may be options for you
To learn more about ovarian or cervical cancer and consult a specialist, schedule an appointment with Thomson Women's Clinic & Cancer Surgery.
Differences between cervical cancer and ovarian cancer
To help you understand the distinction between these two cancers of the reproductive organs, the table below outlines the key differences.
| Cervical cancer | Ovarian cancer | |
|---|---|---|
Origin | Cervix | Ovaries |
Primary cause | HPV infection | Family history or genetic mutations (e.g., BRCA1 or BRCA2) |
Screening tests | HPV and Pap test | CA-125 blood test and pelvic ultrasound |
Common age of onset | Women between 30 and 50 years old | Postmenopausal women (50+ years old) |
Early symptoms | Often asymptomatic in early stages | Vague symptoms (bloating, abdominal pain, or feeling full quickly) |
Prevention | HPV vaccine and regular Pap smears | Risk-reducing surgery for high-risk women |
Treatments | Surgery, radiation, and chemotherapy | Surgery and chemotherapy |
Cervical cancer vs ovarian cancer symptoms
To help you understand the differences between these two conditions and know when to seek medical attention, it is useful to familiarise yourself with the symptoms of each condition.
Cervical cancer symptoms | Ovarian cancer symptoms |
Early-stage cervical cancer usually doesn't cause noticeable symptoms, which is why regular screening is crucial. As the condition progresses, you may experience:
| Ovarian cancer is notorious for having symptoms that are often mistaken for other less serious conditions. Common symptoms include:
|
Since these symptoms can also be caused by other, non-cancerous conditions, experiencing them doesn't necessarily mean that you have cancer. However, if you experience any of these symptoms persistently for more than two weeks, especially if they're affecting your daily life, it's important to seek proper medical evaluation.
If you're not sure if the symptoms you're having are from ovarian or cervical cancer, don't hesitate to schedule an appointment with a women's cancer specialist. At Thomson Women's Clinic & Cancer Surgery, our specialists can perform further assessments and take steps to manage these growths early.
Our women's cancer specialist
Loading...
How are cervical cancer and ovarian cancer diagnosed?
Since the ovaries and cervix are located in different places, different types of tests are used for the diagnosis of these cancers. One big difference is that a doctor can see the cervix directly during an exam, but they can only see the ovaries through imaging tests or surgery because they are completely inside the body.
Nonetheless, the diagnosis of both ovarian and cervical cancer generally begins with a pelvic examination. Here's what you can expect during the diagnostic process:
Cervical cancer diagnosis
To diagnose cervical cancer, your doctor will usually start by carrying out regular cervical cancer screenings using a Pap test. This test can detect most cases of cervical cancer in their early stages, when they are most treatable. The aim of screening is to detect cell changes on your cervix before they become cancerous.
If your Pap test result is abnormal, don't worry – the finding doesn't necessarily mean you have cancer. Further testing helps your doctor get a clearer picture. These tests include:
Initial assessment:
HPV test:
The HPV test examines the cells in your cervix to identify the strains of HPV that are most likely to cause cancer.
Colposcopy and biopsy:
During colposcopy, a specialised magnifying instrument is used to examine the cervix more closely for signs of abnormalities.
If cells look unusual or suspicious, a small sample will be removed (biopsy) and sent to a laboratory for analysis
Tissue removal procedures:
Endocervical curettage:
Your doctor gently scrapes the lining of your cervix with a spoon-shaped tool called a curette
LEEP procedure:
A loop electrosurgical excision procedure (LEEP) is a minor surgical procedure that uses a thin, electrically charged wire loop to remove abnormal tissue from the cervix for examination
If these tests confirm cervical cancer, further tests will establish whether the disease has spread (metastasised). These tests might include:
MRI or CT scans
Blood and urine tests
X-rays of your bladder, rectum, bowels, and lungs
These tests will help your healthcare provider to stage the cancer. Cervical cancer ranges from stage I (least severe) to stage IV (most severe). Staging helps your healthcare provider determine the best treatment plan.
Ovarian cancer diagnosis
On the other hand, an ovarian cancer diagnosis is more challenging because the ovaries are located deep within the pelvis. However, early detection is possible with these approach:
Pelvic examination to checks for unusual masses in your pelvis
Transvaginal ultrasound to help identify abnormal growths or cysts on the ovaries
CA-125 blood test to measures levels of a protein that may be elevated in ovarian cancer
CT or MRI scans to assess the extent of the disease and check for spread to other organs
At Thomson Women's Clinic and Cancer Surgery, our women’s cancer specialists understand that this diagnostic testing can be overwhelming. To help you, our specialist can provide guidance throughout the process, ensuring you understand what is happening and feel supported.
Cervical cancer and ovarian cancer treatments
Cervical and ovarian cancers share some treatment methods, but they often need different kinds of treatment because they are in different places and have different features.
Cervical cancer treatment
Surgery:
Different types of surgery are used to treat cervical cancer, depending on the stage and extent of the disease. If you have an early-stage cervical cancer, and wish to preserve fertility, your provider may recommend a trachelectomy (removal of the cervix while preserving the womb).
However, if the cancer is more advanced, or if fertility preservation is not a concern, a hysterectomy (removal of the uterus and cervix) is usually recommended.
Chemotherapy:
Chemotherapy uses drugs designed to target and remove cancerous cells. These medications work by disrupting cell division, particularly targeting rapidly dividing cancer cells.
Chemotherapy can be used at various stages of cervical cancer – from early stages to shrink tumours before surgery to advanced cases where cancer has spread.
When combined with radiation therapy, chemotherapy kills cancer cells directly and makes them more sensitive to radiation treatment.
Radiation therapy:
Often combined with chemotherapy, radiation therapy is used to treat more advanced stages of cervical cancer.
Brachytherapy, a type of targeted internal radiation therapy, is commonly used alongside external beam radiation as the standard treatment for locally advanced cervical cancer.
Ovarian cancer treatment
Surgery:
The first-line treatment for ovarian cancer usually involves the removal of your reproductive organs and any organ that has cancer on it. Your surgeon may use laparoscopy (a minimally invasive surgery) or laparotomy (open surgery that requires an abdominal incision).
Chemotherapy:
Chemotherapy uses drugs designed to target and remove cancerous cells. These medications work by disrupting cell division, particularly targeting rapidly dividing cancer cells.
Chemotherapy can be used at various stages of ovarian cancer - from early stages to shrink tumours before surgery, to advanced cases where cancer has spread.
Chemotherapy is a drug treatment that uses chemicals to kill fast-growing cells in the body, including cancer cells. Chemotherapy drugs can be injected into a vein or taken by mouth.
Targeted therapy:
This cancer treatment uses drugs to identify and attack specific cancer cells. Targeted therapy works by blocking specific proteins that cancer cells need to grow and divide.
Hormone therapy:
Some ovarian cancers use hormones to grow. This type of therapy blocks hormones, slowing or stopping the growth of cancer.
Thomson Medical's 4-in-1 women screening
To help prevent both cervical and ovarian cancer, early detection is important, as symptoms may not appear until advanced stages. A regular screening can help identify abnormal changes and potential warning signs before they progress. To help prevent these conditions, we offer a 4-in-1 women's screening package, which includes:
Consultation & examination
HPV test
An additional HPV vaccination is also available as an extra protective measure against cervical cancer.
You are not alone
Receiving a cancer diagnosis can feel overwhelming, but remember – you are not alone in this journey. At Thomson Women's Clinic & Cancer Surgery, our specialist provides thorough support, from diagnosis to treatment and follow-up care. We are here to support you with:
Dedicated specialists to guide you through your treatment options.
Regular check-ups and monitoring to ensure you receive the best possible care.
Counselling services to help you and your loved ones cope with the emotional aspects.
We also offer other procedure to help treat cervical and ovarian cancer, which include:
Laparoscopic surgery:
Laparoscopic surgery costs are performed as day surgeries and range from SGD 7,200 to SGD 11,570, depending on whether you choose public or private hospitals.
Colposcopy:
The cost of a colposcopy can vary depending on whether it is performed as day surgery or inpatient surgery, which can cost from SGD 1,200 to SGD 10,400.
However, additional charges may arise for expenses such as pre-surgery consultations, imaging tests (e.g., X-rays or CT scans), medications, and post-surgery follow-up appointments.
Fortunately, there are several programmes in Singapore that can help lower the total cost, such as MediSave, MediShield Life, and Integrated Shield Plans. Each of these offers different levels of coverage depending on your eligibility and insurance arrangements.
This price was last updated in June 2025. Therefore, prices may have changed since then. For more information, contact our medical concierge, who can provide detailed guidance based on your specific situation.
FAQ
Which is more serious, ovarian or cervical cancer?
Both can be serious, but ovarian cancer generally has a higher mortality rate. This is primarily because ovarian cancer is often diagnosed at a later stage, by which time it has usually spread, making treatment more challenging.
In contrast, cervical cancer can usually be detected early through regular screening, leading to better outcomes. Nevertheless, it's important to remember that both conditions can be successfully treated with early detection and proper treatment.
What are signs of ovarian or cervical cancer?
As symptoms of cervical cancer often don't appear until the disease has progressed, regular screening is essential. When symptoms do appear, they may include:
Abnormal vaginal bleeding (between periods, after intercourse or after the menopause)
Unusual vaginal discharge that may be watery, bloody, or have a strong odour
Pelvic pain unrelated to your menstrual cycle
Pain during intercourse
The symptoms of ovarian cancer are often subtle and easily mistaken for common digestive issues.
Persistent abdominal bloating or swelling
Feeling full quickly when eating, even after small meals
Pelvic or abdominal pain that doesn't go away
Urinary urgency or frequency
Unexplained fatigue
Back pain
However, these symptoms can be caused by many non-cancerous conditions. If you experience any of these symptoms for more than two weeks, especially if they are affecting your daily life, it is important to consult your doctor for an evaluation.
Can you have both cervical and ovarian cancer?
It is possible to develop both of these cancers either simultaneously or at different times. However, this is rare because these cancers have different causes, cervical cancer is primarily caused by HPV infection, whereas ovarian cancer is often caused by genetic factors or has an unknown cause.
Are ovarian and cervical cancer hereditary?
The hereditary aspects of the two cancers differ significantly. For example, ovarian cancer has a strong hereditary component.
Individuals with mutations in the BRCA1 or BRCA2 genes are at significantly higher risk.
Having a family history of ovarian, breast, or related cancers also increases the risk.
Conversely, cervical cancer is not usually hereditary.
It is primarily caused by HPV infection rather than genetic factors.
However, family history may play a small role in how your immune system responds to HPV.
Is cervical cancer the same as uterine cancer?
No, they are completely different cancers that affect different parts of the reproductive system.
Cervical cancer:
It develops in the cervix (the lower part of the uterus that connects to the vagina).
It is primarily caused by an HPV infection.
It is highly preventable through vaccination and screening.
Treatment approaches focus on the cervix.
Uterine cancer (endometrial cancer):
It develops in the endometrium (the lining of the uterus).
There are different risk factors, including hormonal influences, obesity and age.
It presents with different symptoms, primarily abnormal uterine bleeding.
It requires different diagnostic and treatment approaches.
It is important to understand these distinctions in order to ensure appropriate screening and care. Regular check-up can help to monitor both areas and detect any abnormalities early on.
Is cervical cancer 100% curable?
Yes, it is highly treatable, particularly if it is found early. When detected early, it can be completely cured with proper treatment. Even advanced cases can benefit significantly from treatment. The key lies in early detection through regular Pap smears and HPV tests, which can identify abnormalities before they develop into cancer.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, schedule an appointment at Thomson Women's Clinic & Cancer Surgery.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Dr Wang Junjie
Obstetrics & Gynaecology (O&G)
Thomson Women's Clinic & Cancer Surgery
English, Mandarin
Prudential, Alliance MediNet


