What is contraception/birth control?
Contraception, commonly known as birth control, refers to the deliberate measures taken to prevent conception. This can encompass a range of methods, including devices, specific sexual practices, chemicals, medications, and surgical procedures designed to intentionally inhibit the occurrence of pregnancy.
What are the major reasons for using contraception?

Empowerment and autonomy:
Contraception empowers individuals, especially women, by providing them with the autonomy to make choices about their reproductive health. This leads to better educational and career opportunities and enhances overall well-being.
Reducing unintended pregnancies:
Access to effective contraception helps in reducing unintended pregnancies, subsequently decreasing the likelihood of unsafe abortions and improving maternal and child health.
Health benefits:
Contraception methods offer health benefits beyond preventing unwanted pregnancies. For instance, hormonal contraceptives can regulate menstrual cycles, reduce menstrual cramps, and alleviate symptoms of conditions like endometriosis.
Economic stability:
Family planning contributes to economic stability by allowing individuals and couples to plan the timing and spacing of their children. This enables better financial planning and allocation of resources.
Preventing sexually transmitted infections (STIs):
Barrier methods, such as condoms, not only prevent pregnancies but also protect against STIs, promoting overall sexual health.
Types of contraception methods
There are several types of contraception methods, each with its own pros and cons. The choice of method depends on factors such as individual preferences, health considerations, and lifestyle. Here are some common types of contraception methods:
Traditional methods
Coitus interruptus or withdrawal
Lactational amenorrhoea method
Rhythm method
Barrier methods
Condoms: These are sheaths worn over the penis (male condoms) or inserted into the vagina (female condoms) to prevent sperm from reaching the egg.
Diaphragms and cervical caps: These are devices that block the cervix, preventing sperm from entering the uterus.
Contraceptive Sponge: A soft, disposable sponge containing spermicide that is placed inside the vagina to block and kill sperm.
Hormonal methods
Birth control pills: Oral contraceptives containing hormones (estrogen and progestin or progestin only) that prevent ovulation and alter cervical mucus to impede sperm.
Birth control patch: A patch applied to the skin that releases hormones to prevent ovulation.
Birth control injection: An injection administered every three months that contains a progestin to prevent ovulation.
Birth control implant: A small rod inserted under the skin of the upper arm that releases hormones to prevent pregnancy for up to three years.
Vaginal ring: A flexible ring inserted into the vagina that releases hormones to prevent ovulation.
Intrauterine devices (IUDs):
Copper IUD: A small, T-shaped device inserted into the uterus that releases copper to prevent fertilisation.
Hormonal IUD: Similar to a copper IUD but releases hormones (usually progestin) to prevent ovulation and thicken cervical mucus.
Permanent methods
Sterilisation: Surgical procedures such as tubal ligation (for women) or vasectomy (for men) that permanently prevent pregnancy.
Emergency contraception
Emergency contraceptive pills (morning-after pill): Pills taken within a few days after unprotected sex to reduce the risk of pregnancy.
What are the most effective contraceptive methods?
The effectiveness of contraceptive methods can vary, and it's important to note that individual preferences, health considerations, and lifestyle factors also play a role in choosing a method. However, based on typical use failure rates (which account for human error and inconsistent use), here is a general ranking of contraceptive methods from most effective to less effective:
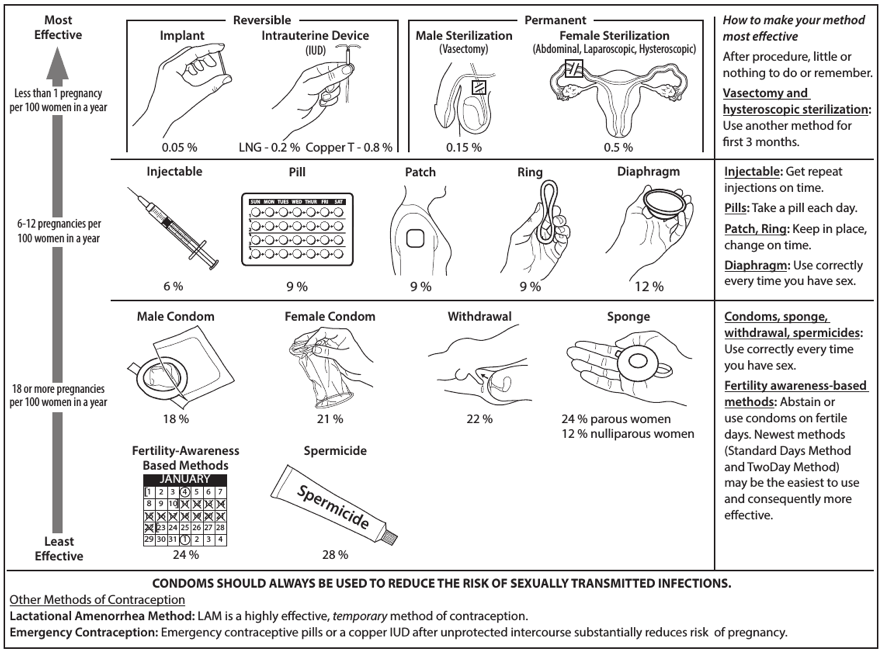
Source: https://www.cdc.gov/reproductivehealth/contraception/mmwr/mec/intro.html
It's important to consult with a healthcare provider to discuss individual preferences and health considerations while determining the most suitable contraceptive method for specific needs. The effectiveness of any method can be influenced by how consistently and correctly it is used.
What are the disadvantages of contraceptives?
Side effects:
Many contraceptive methods, especially hormonal ones like birth control pills, patches, and injections, can cause side effects. These may include nausea, headaches, weight gain, mood changes, and changes in libido. Not all individuals experience these side effects, and they can vary from person to person.
Health risks:
- Some hormonal contraceptives may pose certain health risks, especially for individuals with pre-existing conditions. For example, women over 35 who smoke are at a higher risk of cardiovascular issues when using hormonal birth control methods.
Inconvenience:
- Some contraceptive methods, such as birth control pills or patches, require strict adherence to a schedule. This can be inconvenient for individuals with busy lifestyles or those who may have difficulty remembering to take medication regularly.
Variability in effectiveness:
- The effectiveness of some contraceptive methods can vary depending on factors such as consistency of use, timing, and individual health. User-dependent methods, like condoms or spermicides, may have higher failure rates if not used correctly.
Cost:
The cost of some contraceptive methods, particularly certain long-acting reversible contraceptives (LARCs) or newer hormonal options, may be a barrier for some individuals. Access to affordable and effective contraception can be a challenge for certain populations.
Fertility return delay:
- After discontinuing certain hormonal contraceptives, it may take some time for fertility to return to normal. This delay can be a concern for individuals who wish to conceive soon after stopping contraception.
Mood and libido changes:
- Hormonal contraceptives can sometimes affect mood and libido, leading to changes in sexual desire and overall well-being. This can vary among individuals, and not everyone experiences these effects.
Method failure:
- No contraceptive method is 100% effective. There is always a small risk of method failure, leading to unintended pregnancies. This risk is generally higher with user-dependent methods or those that require strict adherence.
FAQ
What contraceptive is the best?
The "best" contraceptive method depends on individual preferences, health considerations, and lifestyle. There is no one-size-fits-all solution, and the effectiveness of a contraceptive method can vary from person to person. It's essential to consult with a healthcare professional to determine the most suitable option based on your specific needs.
Which birth control has the lowest failure rate?
The birth control implant has the lowest failure rate among all contraceptive methods.
What birth control doesn't harm your body?
All forms of birth control may have potential side effects or risks, and what may be suitable for one person might not be ideal for another. It's important to recognise that the concept of harm can vary from person to person, and the decision about which birth control method to use should be based on individual health considerations, preferences, and lifestyle. Please consult your doctor for advice.
What is the birth control that is 100% effective?
There is no birth control method that is 100% effective. While some methods, such as sterilisation procedures like tubal ligation or vasectomy, are highly effective, there is still a small chance of failure. Additionally, human error, improper use, or unexpected complications can reduce the effectiveness of any birth control method.
Does pulling out prevent pregnancy?
The "pulling out" method, also known as withdrawal or the withdrawal method, involves the man withdrawing his penis from the vagina before ejaculation to prevent sperm from entering the woman's reproductive system. While it can reduce the risk of pregnancy, it is not considered a highly effective method.
The withdrawal method is not as reliable as other forms of contraception, such as condoms or hormonal methods. One of the main reasons is that it relies on perfect timing and self-control, and there is a risk of pre-ejaculate (pre-cum) containing sperm, which can still lead to pregnancy.
Should I take Plan B if he didn't finish?
Taking emergency contraception, such as Plan B, is designed to prevent pregnancy after unprotected sex or contraceptive failure. However, it's important to note that the withdrawal method (pulling out) is not foolproof, as pre-ejaculate (pre-cum) can contain sperm, even if a man doesn't fully ejaculate.
If there is a concern about the possibility of pregnancy and you want to take precautions, using emergency contraception like Plan B may be an option. It works by preventing or delaying ovulation and inhibiting fertilisation.
Who should use contraceptives/birth control?
Couples who desire to plan the timing and spacing of their children:
- They may use contraception to achieve their family planning goals, ensuring that they are fully emotionally, financially, and physically prepared for the responsibilities of parenthood.
Couples post-childbirth:
- Couples who have recently given birth and are not ready for another pregnancy may use contraception to allow the mother's body time to recover and to plan the spacing of their children appropriately.
Couples facing economic challenges:
- Couples facing financial instability may use contraception to manage their family size, ensuring that they can provide adequate care and attention for their existing children while maintaining a stable economic environment.
Women with menstrual health issues:
- Women experiencing irregular menstrual cycles, painful periods, or conditions like polycystic ovary syndrome (PCOS) may use hormonal contraception to regulate their cycles, alleviate symptoms, and improve overall reproductive health.
Individuals with health concerns:
Some individuals may have health conditions that make pregnancy risky for them or the potential child. In such cases, healthcare providers might recommend specific contraception methods to safeguard the health of both the individual and the future child.
People at risk of sexually transmitted infections (STIs):
Condoms, in addition to preventing pregnancies, act as a barrier against sexually transmitted infections. Individuals engaging in sexual activities with new or multiple partners may use condoms to reduce the risk of contracting or spreading STIs.
Individuals pursuing education or careers:
Individuals focused on educational and career pursuits may choose to delay parenthood until they feel more established in their professional lives. Contraception allows them to control the timing of family expansion.
Individuals wanting to avoid stereotypes and gender roles:
Contraception empowers individuals, especially women, to break free from traditional gender roles and stereotypes. It enables women to make choices about their reproductive health, education, and career without being confined by societal expectations.
What causes the contraceptives to fail?
Inconsistent or incorrect use:
- One of the most significant reasons for contraception failure is inconsistent or incorrect use. Forgetting to take birth control pills, not using condoms properly, or failing to follow the prescribed instructions for other contraceptive methods can reduce their effectiveness.
Missed pills or late injections:
- For hormonal methods such as birth control pills or injections, missing doses or not taking them at the same time every day can compromise their effectiveness. Similarly, if individuals are late for receiving contraceptive injections, it may lead to a decrease in protection against pregnancy.
Barrier method issues:
- Condoms, both male and female, are barrier methods that rely on proper usage. Condoms can break or slip off if not used correctly, and using expired condoms can also increase the risk of failure.
Drug interactions:
- Some medications, such as certain antibiotics or anticonvulsants, can interact with hormonal contraceptives, reducing their effectiveness. It's important to consult a healthcare professional when taking medications that may interfere with contraception.
Health conditions:
Certain health conditions or gastrointestinal issues, such as vomiting or diarrhea, can affect the absorption of contraceptive pills, rendering them less effective. Individuals with certain medical conditions may also be advised against using specific methods of contraception.
Storage and expiration:
- Contraceptive methods have expiration dates, and if they are used after this date, their effectiveness may be compromised. Proper storage is also crucial to maintain the integrity of the contraceptive method.
Sperm viability:
- Contraceptive methods that rely on preventing sperm from reaching an egg (e.g., spermicides or diaphragms) may not be 100% effective, as sperm can sometimes still reach and fertilise an egg.
Human error:
Even with the best intentions, human error can occur. Forgetting to use contraception during sexual activity or miscalculating fertile periods in natural family planning methods can result in unintended pregnancies.
Lack of education and communication:
- Inadequate education about contraceptive methods and poor communication between sexual partners can lead to misunderstandings or mistakes in using contraception effectively.
For more information, contact us:
Thomson Specialists (Women's Health)
- Paragon (female doctor): +65 6735 0300
- Woodleigh: +65 8684 0153
Thomson Women's Clinic
- Bukit Batok: +65 6569 0668
- Choa Chu Kang: +65 6893 1227
- Jurong: +65 6262 8588
- Punggol: +65 6243 6843
- Sembawang: +65 6753 5228
- Sengkang: +65 6388 8125
- Serangoon (female doctor): +65 6382 3313
- Tampines: +65 6857 6266
- Tiong Bahru: +65 6276 1525
Notice
The range of contraceptive options may vary between Thomson Women's Clinic (TWC) locations. Please contact your preferred TWC branch directly to enquire about the current availability of specific contraceptive methods.
Request an AppointmentDr Ryan Lee Wai Kheong
Obstetrics & Gynaecology (O&G)
Thomson Specialists Woodleigh (Women's Health)
English, Mandarin
Adept, MHC, HSBC, Alliance MediNet and 1 other

