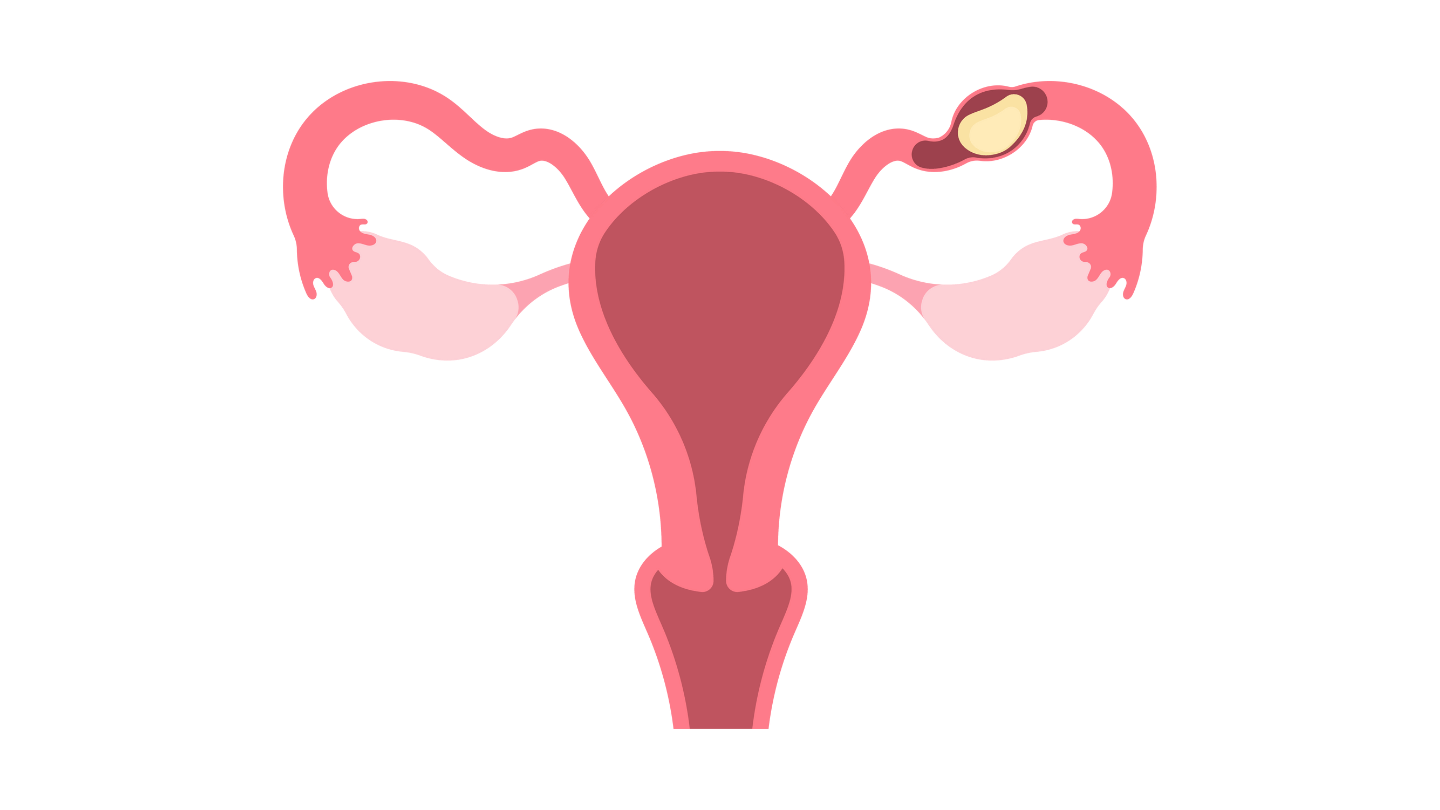
What is an ectopic pregnancy?
An ectopic pregnancy refers to a rare occurrence where the fertilised egg implants and grows outside the uterus, such as the fallopian tube (tubal pregnancy). Ectopic pregnancies may also happen in the ovary, abdominal cavity or cervix.
This condition is relatively rare, with 5 to 7 out of every 1,000 pregnancies being ectopic pregnancies. However, if not caught and treated early, it could pose a serious risk or mortal threat to maternal health during the first trimester (3 months) of pregnancy.
Ectopic pregnancy: symptoms & signs
Recognising the symptoms of an ectopic pregnancy could help prevent severe complications and future fertility issues.
Early symptoms generally start 6-8 weeks after the last normal menstrual period, these include:
Sharp or stabbing pain:
A sharp or stabbing pain, typically on one side of the abdomen or pelvis. This may come and go, or vary in intensity.
Urinary or bowel symptoms:
Pain or discomfort during urination or bowel movements.
Vaginal bleeding:
Unusually light or heavy bleeding different from your usual menstrual period.
Other pregnancy symptoms:
Other pregnancy symptoms such as breast tenderness and nausea.
Symptoms of an ectopic pregnancy rupture are:
Shoulder pain:
Internal bleeding could irritate the diaphragm, causing pain at the tip of the shoulder.
Dizziness:
Weakness, dizziness or fainting could be caused by severe internal bleeding and low blood pressure. This should be treated as an emergency and requires immediate medical attention.
If you experience symptoms of an ectopic pregnancy rupture, please seek immediate medical attention, as your life could be at risk.
What causes ectopic pregnancy?
Ectopic pregnancies are generally caused by factors that prevent a smooth journey for the fertilised egg through the fallopian tube to the uterus. This includes several factors, such as:
Endometriosis:
A condition characterised by scarring in the pelvis, which, in turn, affects the fallopian tubes.
Tobacco smoking:
Smoking can cause damage to tissues in the body, including the fallopian tubes.
Maternal age over 35:
Women aged between 35 to 44 are at higher risk of ectopic pregnancy.
Previous ectopic pregnancy:
Having had an ectopic pregnancy increases your risk of another.
Infections:
Infections, such as pelvic inflammatory disease (PID) and other sexually transmitted infections (STIs) can damage the fallopian tubes.
History of tubal surgery or pelvic surgery:
Prior reproductive surgeries could cause tissue scarring and lead to implantation issues.
Contraception:
Although rare, if a pregnancy occurs despite contraception with an intrauterine device (IUD) or tubal ligation, it will likely be an ectopic pregnancy.
Hormonal imbalance:
Certain hormonal conditions, such as hypothyroidism or polycystic ovarian syndrome (PCOS) can adversely affect the fallopian tube’s normal function, increasing your risk of ectopic pregnancy.
To discuss which procedure would be most suitable for your condition, schedule a consultation with Thomson Fertility Centre. Our fertility specialist can provide more information about ectopic pregnancy.
What increases your risk of ectopic pregnancy?
While ectopic pregnancies can happen to anyone, certain factors can increase your risk. Understanding these can help with early diagnosis and prompt medical care.
Common risk factors include:
Previous ectopic pregnancy:
Having one increases the likelihood of recurrence.
Pelvic inflammatory disease (PID):
Often caused by infections like chlamydia or gonorrhoea, which can damage the fallopian tubes.
Tubal surgery:
Procedures such as tubal ligation or surgery to correct blocked tubes may increase the risk.
Fertility treatments:
In vitro fertilisation (IVF) and other assisted reproductive techniques carry a slightly higher risk.
Smoking:
Smoking may affect the function of the fallopian tubes and increase ectopic pregnancy risk.
Endometriosis:
This condition can cause scarring in or around the fallopian tubes, making normal implantation more difficult.
Use of an intrauterine device (IUD):
While rare, pregnancy occurring with an IUD in place is more likely to be ectopic.
If you have any of these risk factors and suspect you might be pregnant, it's important to seek medical attention early. Early detection can help reduce complications and protect your fertility.
Obstetrician-gynaecologist in Singapore
Loading...
How is an ectopic pregnancy diagnosed?
Accurately diagnosing an ectopic pregnancy involves a series of blood and imaging tests to confirm the presence and location of the ectopic pregnancy. This is usually done by an obstetrician-gynaecologist.
Medical history and physical examination
Your doctor will ask about your medical past and current symptoms, including–but not limited to–vaginal bleeding or previous ectopic pregnancies, while physical examinations might include assessing for tenderness or pain in the lower abdomen, or signs of internal bleeding.
Transvaginal ultrasound
Used for confirming an ectopic pregnancy through identifying structural abnormalities or abnormal masses, transvaginal ultrasounds work by inserting a small, lubricated probe called a transducer into the vagina to visualise pelvic organs, including the uterus, ovaries and fallopian tubes.
Blood tests
Blood tests may be carried out, including one on human Chorionic Gonadotropin (hCG) levels, which are typically produced during pregnancy. When monitored over time, ectopic pregnancies present a slower or lower rise in hCG levels compared to normal pregnancies.
MRI (magnetic resonance imaging)
An additional magnetic resonance imaging test may be recommended when transvaginal ultrasound results are inconclusive. This 30-60 minute test can provide detailed images of the tissues, and helps the gynaecologist identify the exact location of the ectopic pregnancy.
Ultimately, a thorough diagnosis helps the gynaecologist differentiate between other conditions that present with similar symptoms, such as a miscarriage or an ovarian cyst rupture. Early diagnosis is crucial for timely intervention to prevent further complications.
What are the complications of ectopic pregnancy?
Rupture of the fallopian tube
One of the most severe complications of ectopic pregnancy involves the embryo growing and causing the fallopian tube to stretch and rupture, leading to internal bleeding.
Haemorrhage and shock
Internal bleeding from the rupture of the fallopian tube can cause significant blood loss, leading to haemorrhagic shock: a life-threatening condition caused by insufficient blood flow to the vital organs, including the brain and heart.
Infertility
Fertility can be affected by damage to the fallopian tube or other reproductive organs, as ectopic pregnancy surgery may result in the removal of a portion of the fallopian tube, reducing a woman's ability to conceive naturally.
Chronic pelvic pain
The resulting scarring to the fallopian tubes or surrounding tissues may result in chronic pelvic pain. Scar tissue can form, causing discomfort or pain during intercourse, menstruation, or daily activities.
Psychological impact
People can be significantly affected by the psychological impact of ectopic pregnancy. Feelings of grief, sadness, anxiety, or depression are common and may require counselling or support.
Recurrence
Some women who have had one ectopic pregnancy are at higher risk of having another, especially if certain causes, such as pelvic inflammatory disease or tubal damage, persist.
How is an ectopic pregnancy treated?
The treatment for an ectopic pregnancy largely depends on the size and location of the implantation, with the main aim to preserve the patient’s health and fertility. If an ectopic pregnancy has ruptured, an emergency procedure may be required.
Medical management
- Methotrexate injection:
-
- Methotrexate generally works by mitigating the growth of rapidly dividing cells and dissolving existing cells in an ectopic pregnancy.
- One dose is administered via injection, which is then monitored closely with serial blood tests (hCG levels) and ultrasounds.
Surgical management
There are 3 main methods to effectively manage an ectopic pregnancy:
- Laparoscopic surgery:
-
- Laparoscopic surgery is a minimally invasive alternative to traditional surgeries.
- It involves the use of keyhole-sized incisions, a miniature camera (laparoscope), and surgical instruments to access and remove the ectopic pregnancy. This allows for a shorter hospital stay and lower risk of complications.
- Salpingectomy:
-
- A salpingectomy involves the permanent surgical removal of the affected fallopian tube in the event of significant damage or a rupture.
- Salpingostomy:
-
- A salpingostomy refers to the surgical removal of the ectopic pregnancy while preserving the fallopian tube.
- This is recommended if the ectopic pregnancy is small and the fallopian tube is generally healthy.
Contraception
After your treatment, your gynaecologist may prescribe contraceptives until it is safe to conceive again. This will typically be after a few menstrual cycles and clearance from your doctor.
FAQ
Where can ectopic pregnancy occur?
While ectopic pregnancies most commonly occur in the fallopian tubes 95% of the time, they can also implant in other locations, including:
- Ovaries
- Abdominal cavity
- Cervix
Can a baby be saved in an ectopic pregnancy?
Unfortunately, the foetus cannot be saved in an ectopic pregnancy. The main treatment involves removing the pregnancy before it grows too large or causes a rupture.
Can a woman still have a baby with an ectopic pregnancy?
Yes, there is a very low risk of recurrence for an ectopic pregnancy. Most women who have experienced ectopic pregnancy and treatment are able to achieve a successful pregnancy in the future.
Will my pregnancy test be positive even if it is an ectopic pregnancy?
Yes, the results will still be positive even with an ectopic pregnancy. They also present with usual signs of pregnancy, such as missed periods and breast tenderness.
Can ectopic pregnancy go away on its own?
In some instances, an ectopic pregnancy can shrink on its own and leave the body naturally. However, it is best to get the right medical attention to properly manage your condition and prevent complications.
Does your belly grow with an ectopic pregnancy?
Unlike a typical pregnancy, your belly will not grow with ectopic pregnancy, as the foetus will not have space to expand and grow normally.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, please consult a specialist by requesting an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
