What are uterine fibroids?
Fibroids, also known as leiomyomas or uterine fibroids, are non-cancerous growths that develop from the connective tissue and muscle walls of the uterus (womb), the part of your body where the baby develops. Uterine fibroids can vary in size, from tiny pea-sized growths to large masses the size of a grapefruit.
They can be single or multiple, and they can develop in different parts of the uterine wall. It's possible for an individual to be unaware that they have these tumours, as the majority of uterine fibroids are small and cause no symptoms, unless they're larger than 5 cm or if there are multiple fibroids.
Types of fibroids
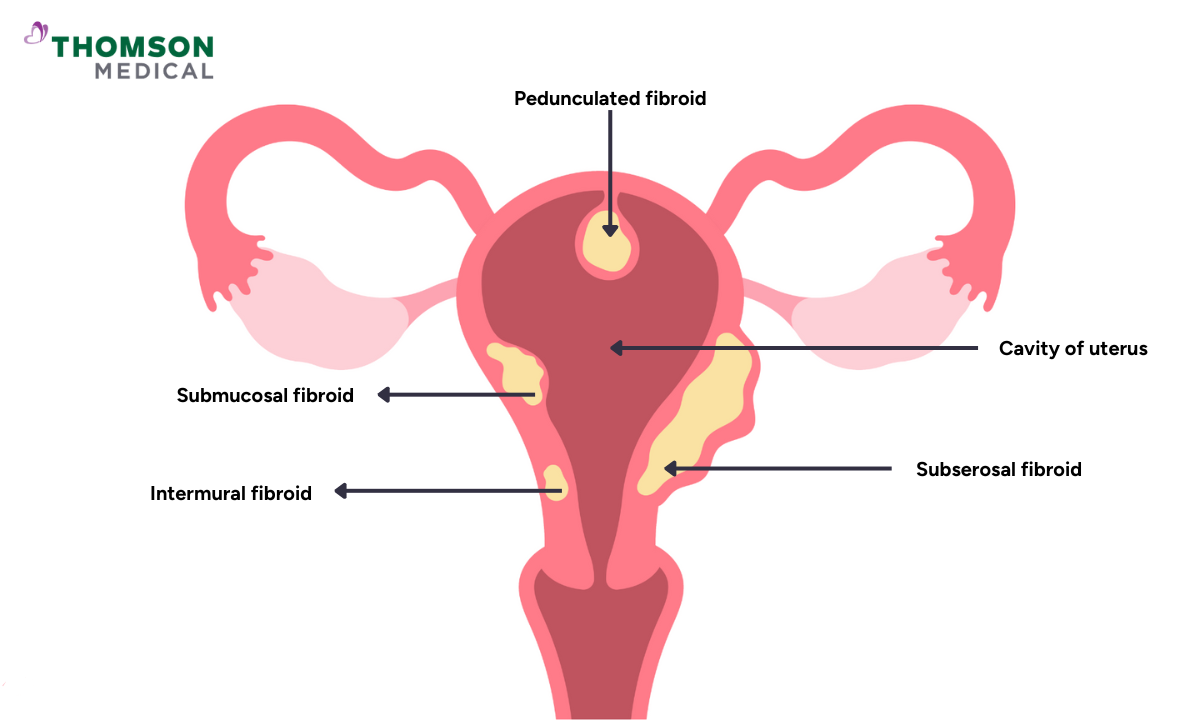
Depending on their location, there are four types of fibroids:
Intramural fibroids
This is the most common type of fibroid, and it grows inside the muscular wall of the uterus. This growth can enlarge the uterus and cause symptoms such as heavy menstrual bleeding and pelvic pain.
Subserosal fibroids
Located on the outer surface of the uterus, this type of growth can press on nearby organs such as the bladder or bowel, causing discomfort.
Submucosal fibroids
These fibroids grow under the inner lining of the uterus and often cause heavy menses and can lead to infertility problems or repeated miscarriages.
Pedunculated fibroids
This is the least common type of fibroid; it's attached to the wall of the uterus by a stalk or stem. It can cause pain, bleeding, and, in some cases, pregnancy complications.
What are the symptoms of uterine fibroids?
Fibroids can cause a range of symptoms depending on their size, number, and location in the uterus. Common symptoms that can be caused by these growths include
Prolonged menstrual bleeding
Fibroids can cause menstrual bleeding to last longer than usual, increasing the risk of heavy blood loss. These conditions can lead to fatigue and an increased risk of iron deficiency anaemia (loss of blood cells and low blood count).
Pelvic pressure
Larger fibroids can press against the surrounding tissue, causing a persistent feeling of discomfort, pain during sex, heaviness, or fullness in the lower abdomen.
Frequent urination
If uterine fibroids are close to the bladder, they can put pressure on these organs and cause an increased need to urinate or urinary retention (where your bladder doesn't empty completely).
Abdominal bloating
Enlargement of the uterus due to fibroid growth can cause noticeable swelling or a bulge in the abdomen, often mistaken for weight gain.
Constipation
Fibroids pressing against the rectum or bowel can interfere with normal bowel movements, causing them to be difficult or infrequent.
Infertility
Submucosal fibroids, or large intramural fibroids, can cause fertility problems by distorting the uterine cavity or blocking the fallopian tubes (where fertilisation takes place).
Depending on the severity of the fibroids, symptoms may vary, with some people experiencing severe abdominal discomfort while others may have no noticeable symptoms. To help manage this condition, request an appointment with Thomson Medical for personalised advice tailored to your needs.
Uterine fibroids causes
While the exact cause of uterine fibroids remains unclear, there are several risk factors that are known to be associated with an increased risk of fibroid growth, including:
Age
Fibroids are most commonly found in women between the ages of 30 and 40.
Family history
If a family member has had or currently has a fibroid, the likelihood of developing one is increased.
Hormonal influence
Increased progesterone and oestrogen hormone levels during the menstrual cycle can lead to the development of fibroids.
Obesity
Excess body weight increases the risk of fibroids.
Diet
A diet high in red meat and processed foods and low in vegetables, fruit and dairy products.
Reproductive history
Early onset of menstruation and no pregnancy (nulliparity) are associated with a higher risk.
Women who have fibroids smaller than 5 cm can still have a normal pregnancy without complications. However, if the fibroids are larger than 5 cm, or if there are multiple growths of fibroids, there's an increased risk of pregnancy complications such as miscarriage or premature labour, and the baby may not be delivered in the correct position.
How are fibroids diagnosed?
Fibroids are often discovered during a pelvic examination, as the doctor may notice irregularities in the shape of the uterus. To further confirm the presence of these growths and assess their size and location, there are several tests that can be performed, which include:
Clinical assessment
Your doctor will ask you about symptoms, history of heavy periods, pelvic pain, and family medical history of fibroids or related conditions. On a physical exam, your uterus may be found to be enlarged when feeling for a mass in the abdomen.
Pelvic examination
A healthcare provider may perform a pelvic exam to feel for any abnormalities in the size or shape of the uterus.
Ultrasound imaging
Abdominal or transvaginal ultrasounds can help visualise the size, number, and location of uterine fibroids.
Magnetic resonance imaging (MRI)
- MRI scans may be used to provide detailed imaging of the uterus and fibroids, especially in cases where ultrasound results are inconclusive or further evaluation is needed.
Treatment options
Fibroid treatment can help relieve fibroid symptoms while preserving fertility and improving quality of life. Your choice of treatment will depend on the severity of your symptoms, fibroid size, and your plans for future pregnancy. There are several treatment plans for fibroids, including:
Conservative treatment
Conservative management is suitable for people with fibroids that cause no or minimal symptoms. This approach avoids invasive procedures and relies on watchful waiting and monitoring. This means you'll need to have regular check-ups so that your healthcare provider can monitor any changes in the size and symptoms of your fibroids.

Medical treatment
Medical treatments for fibroids aim to reduce symptoms such as heavy, painful periods and pelvic pain or tenderness. They usually do not shrink the fibroids but only manage the symptoms. Here are some common medical treatments that may be used, such as:
Hormonal birth control pills
It regulates your hormone levels to help manage heavy periods and pain.
Antifibrinolytic medications (e.g., tranexamic acid)
This medication slows down menstrual bleeding by aiding clot formation; it's effective for immediate symptom control.
Antifibrinolytics should not be combined with hormonal contraceptives without medical advice because of the risk of blood clots.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Medications such as mefenamic acid or naproxen reduce menstrual cramps and vaginal bleeding.
GnRH analogues (e.g., Lucrin)
This medicine temporarily shrinks the fibroids and stops menstrual periods for up to six months. However, they may grow back after the medicine is stopped. Hormone treatments such as injectable GnRH analogues may cause temporary menopause-like symptoms.
Levonorgestrel-releasing IUD (e.g., Mirena)
Intrauterine devices (IUDs) slowly release progesterone-like hormones to reduce heavy vaginal bleeding during periods; they are highly effective and localised with minimal systemic effects.
Iron supplements
Treatment for iron deficiency caused by abnormal bleeding during heavy periods.
It's important for you to inform your gynaecologist about any new or worsening symptoms to ensure accurate treatment. Request an appointment to see our women's health specialist for personalised care tailored to your needs.
Surgical treatment
Surgery is an invasive procedure that is usually reserved for when you have severe symptoms, the fibroids are not responding to treatment, or you want to get pregnant, but the fibroids are affecting the uterine cavity. There are several surgical procedures that can be performed, including:
Myomectomy
Myomectomy is an invasive procedure that removes the fibroids while preserving the uterus. It is ideal for women who want to become pregnant in the future or to relieve symptoms without removing the uterus.
Risks include the possibility of recurrence (10-25%) and delayed pregnancy (at least six months). There are several types of myomectomy procedures, including:
Abdominal myomectomy, which is an open surgery for multiple or larger fibroids.
A laparoscopic myomectomy is a minimally invasive surgery that involves small incisions.
Transcervical resection of myoma (TCRM), which is used for hysteroscopic removal of submucosal fibroids inside the uterus.
Hysterectomy
Hysterectomy is a major operation involving the complete removal of the uterus. It is more suitable for people with completed family plans, multiple large fibroids, or recurrent fibroids after myomectomy. It is also recommended for post-menopausal women.
It provides a permanent solution to heavy bleeding and pressure symptoms but does not eliminate the possibility of pregnancy.
Alternative treatments
For those seeking non-surgical, less invasive approaches:
Uterine artery embolisation (UAE)
This procedure, also known as uterine fibroid embolisation, blocks the blood vessel that supplies blood flow to fibroids, causing them to shrink and relieving pain. Pregnancy is generally not recommended after this procedure.
Magnetic resonance-guided focused ultrasound (MRgFUS)
Non-invasive destruction of fibroids using focused sound waves under MRI guidance.
Effective in relieving symptoms and reducing fibroids.
Endometrial ablation or resection
Removal of the uterine lining to control heavy bleeding.
Not suitable for those wishing to avoid adverse effects on future fertility.
It's important for you to inform your gynaecologist about any new or worsening symptoms to ensure accurate treatment. Request an appointment to see our women's health specialist for personalised care tailored to your needs.
Complications of uterine fibroids
While fibroids are generally benign (non-cancerous), they can lead to:
Menstrual irregularities
Heavy bleeding, prolonged menstrual periods and signs of anaemia.
Chronic pain
Persistent discomfort caused by pelvic pressure or degeneration of a fibroid.
Degeneration
Fibroids can outgrow their blood supply, leading to degeneration of the fibroid tissue, which can cause severe pain and discomfort.
Malignancy
While fibroids are typically non-cancerous, there is less than a 1% chance they could become malignant fibroid tumours (leiomyosarcoma).
Complications during pregnancy
Increased risks of miscarriage, preterm labour, and delivery by caesarean section. Sometimes the pregnancy doesn't even happen because of blockage of fallopian tubes.
Psychological effects
Impact on mental health due to chronic symptoms. fertility challenges and impact on body image.
A personalised approach is essential to ensure optimal outcomes, particularly if fertility preservation is a concern. Request an appointment with our specialists at Thomson Medical today.
FAQ
Can fibroids become malignant?
Although fibroids are usually benign (non-cancerous) growths, in rare cases they can become malignant and become cancerous. The risk of fibroids developing into malignant tumours called leiomyosarcomas is extremely low, estimated to be less than 1%.
When should you seek treatment?
Seek professional advice if you are experiencing:
Heavy or prolonged menstrual bleeding.
Abdominal pain or pressure in the pelvis.
Pain during sex.
Difficulty conceiving.
Urinary or bowel problems.
Can you live normally with fibroids?
Yes, you can. Many women with fibroids lead normal lives without significant disruption to their daily activities. This is especially true for small fibroids (less than 5 cm) that cause minimal or no symptoms.
Can fibroids shrink on their own?
In some cases, fibroids may shrink after the menopause due to a decrease in oestrogen and progesterone levels, but others may continue to grow or cause symptoms.
Can uterine fibroids affect pregnancy?
Yes, certain fibroids can interfere with conception and pregnancy, especially those that distort the uterine cavity or block the fallopian tubes.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
- Paragon (female doctor): +65 6735 0300
- Woodleigh: +65 8684 0153
Thomson Women's Clinic (TWC)
- Bukit Batok: +65 6569 0668
- Choa Chu Kang: +65 6893 1227
- Jurong: +65 6262 8588
- Punggol: +65 6243 6843
- Sembawang: +65 6753 5228
- Sengkang: +65 6388 8125
- Serangoon (female doctor): +65 6382 3313
- Tampines: +65 6857 6266
- Tiong Bahru: +65 6276 1525
Dr Ryan Lee Wai Kheong
Obstetrics & Gynaecology (O&G)
Thomson Specialists Woodleigh (Women's Health)
English, Mandarin
Adept, MHC, HSBC, Alliance MediNet and 1 other

