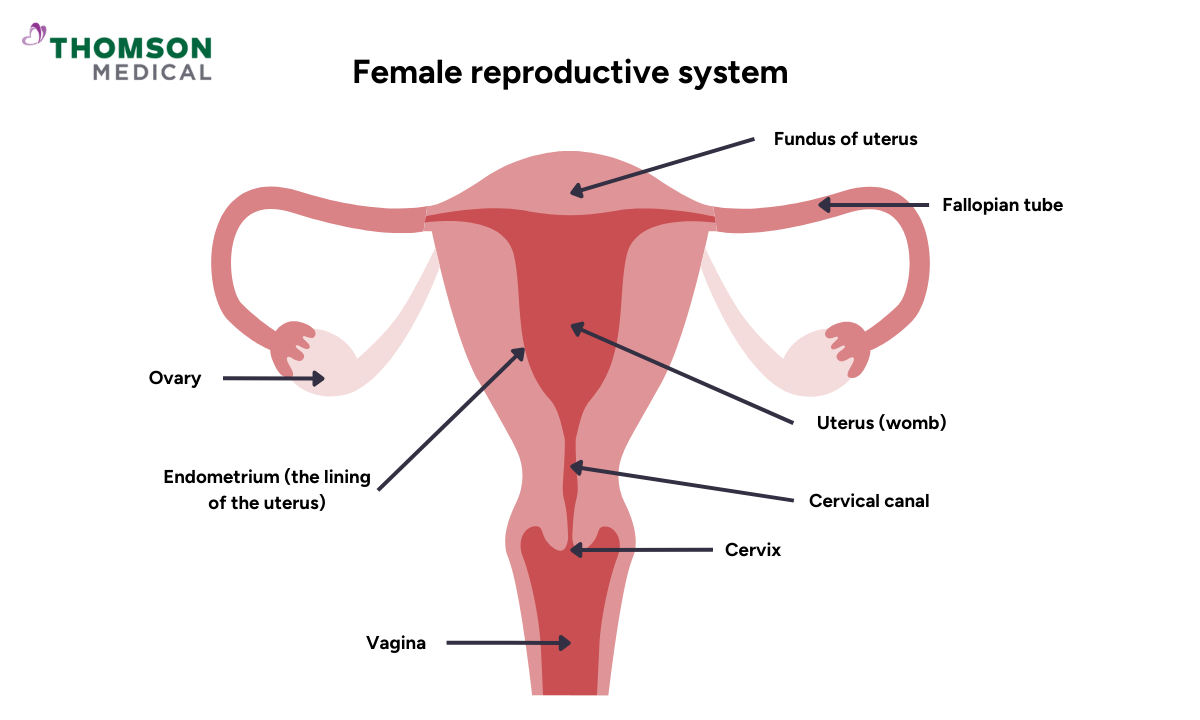
The female reproductive system is comprised of several key structures, including the ovaries, fallopian tubes, uterus, cervix, and vagina (refer to the illustration below). Gynaecological cancers, which are cancerous tumors originating in any of these components, represent a significant health concern.
According to data from the Singapore Cancer Registry, during the period from 2017 to 2021, cancers of the uterus, ovary, and cervix were identified as the fourth, sixth, and tenth most prevalent cancers, respectively, among women in Singapore.
Gynaecological cancer screening plays a crucial role in the early detection and prevention of cancers affecting the female reproductive system.
In this article, we will look at the screenings for:
Cervical cancer
Ovarian cancer
Endometrial cancer
Cervical cancer screening
Pap smear test
According to the Ministry of Health (MOH), all women who have ever engaged in sexual intercourse should undergo cervical cancer screening starting at the age of 25.
In Singapore, the Pap smear is a routine screening test available in polyclinics and private clinics.
HPV testing
Human Papillomavirus (HPV) testing is often used in conjunction with Pap smears.
HPV vaccination is a preventive measure, typically administered to girls between the ages of 9 and 14.
Ovarian cancer screening
CA-125 blood test
CA-125 is a protein that may be elevated in the presence of ovarian cancer.
However, CA-125 levels can be influenced by various factors, leading to limited reliability.
Pelvic ultrasound
Pelvic ultrasound involves detailed images of the ovaries to visualise any ovarian masses with suspicious features of cancer such as solid areas, ascites, or bilateral cysts.
Endometrial cancer screening
Endometrial cancer is a type of cancer that begins in the lining of the uterus, known as the endometrium.
Endometrial biopsy
Recommended for women experiencing abnormal vaginal bleeding or those at higher risk of endometrial cancer such as obesity, diabetes, or polycystic ovarian syndrome.
Helps diagnose endometrial cancer by examining a small tissue sample from the uterine lining.
Hysteroscopy, dilation, and curettage can be performed as an alternative to endometrial biopsy as an investigation of abnormal vaginal bleeding.
Transvaginal ultrasound
Imaging technique that allows visualisation of the ovaries for abnormalities.
Not recommended as a standalone screening tool due to its limited sensitivity and specificity.
FAQ
Why is early detection important in gynaecological cancers?
Early detection of gynaecological cancers significantly increases the chances of successful treatment and cure. Regular screenings help identify abnormalities or cancerous cells at an early stage when intervention is most effective.
Which cancers are screened for in routine gynaecological exams?
Routine gynaecological exams typically screen for cervical, ovarian, and uterine (endometrial) cancers. Vaginal and vulvar cancers are often assessed during pelvic exams.
When should I start cervical cancer screening?
It is recommended that women who are sexually active begin cervical cancer screening at the age of 25.
How often should I undergo cervical cancer screening?
It is advised that women between the ages of 25 and 29 undergo a Pap test every three years. This recommendation does not apply to women with a history of previous abnormal Pap smears who are following up with a gynaecologist.
For women aged 30 and older, they are recommended to get a Human Papillomavirus (HPV) test every five years.
Can ovarian cancer be detected early?
Early detection of ovarian cancer is challenging, and there is no routine screening test with high accuracy. Awareness of symptoms, such as bloating, pelvic pain, and changes in bowel habits, is crucial for early diagnosis.
What are the symptoms of gynaecological cancers?
Symptoms vary depending on the type of cancer but may include abnormal vaginal bleeding, pelvic pain or pressure, changes in bowel or bladder habits, and unexplained weight loss. However, many women with early-stage cancers may not experience any symptoms.
When should women start and stop gynaecological cancer screenings?
Screening guidelines may vary based on factors like age, risk factors, and personal medical history. It is crucial to discuss individualised screening plans with healthcare providers. Generally, screenings may start in the early 20s and continue until the mid-60s.
Can gynaecological cancers be prevented?
Some risk factors, like HPV infection, can be addressed through vaccination. Additionally, lifestyle factors such as maintaining a healthy weight, not smoking, and using protection during sexual activity can potentially contribute to reducing the risk of gynaecological cancers.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations based on your medical conditions, request an appointment with Thomson Medical.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Dr Ryan Lee Wai Kheong
Obstetrics & Gynaecology (O&G)
Thomson Specialists Woodleigh (Women's Health)
English, Mandarin
Prudential, Great Eastern, Adept, MHC and 4 others

